Degenerative changes, especially those resulting from accidental injuries affecting the spine, may result in pain, reduced mobility, postural abnormalities or, at worst, paralyses and sensory disorders.
While the injuries that young people present with are almost always the result of a serious accident, older patients are more likely to present with spontaneous vertebral body fractures that are associated with osteoporosis, or with herniations of degeneratively altered intervertebral discs or arthrosis in the small vertebral articulations. In rare cases, inflammation, tumours or metastases may bring about similar afflictions. The connection to the pelvis (comprising the sacral and coccygeal bones along with the sacroiliac joint) is an important, and often similarly affected, region of the lower spine, for which reason pelvic changes are addressed by the same team.
Our treatment plans are predicated on the use of state-of-the-art technology to achieve an accurate diagnosis, and they emphasise first and foremost a personalised approach to treating your underlying disorders. With that in mind, this page is divided into subsections to help you navigate to the information that best describes the treatment programme that is most applicable to your particular case.
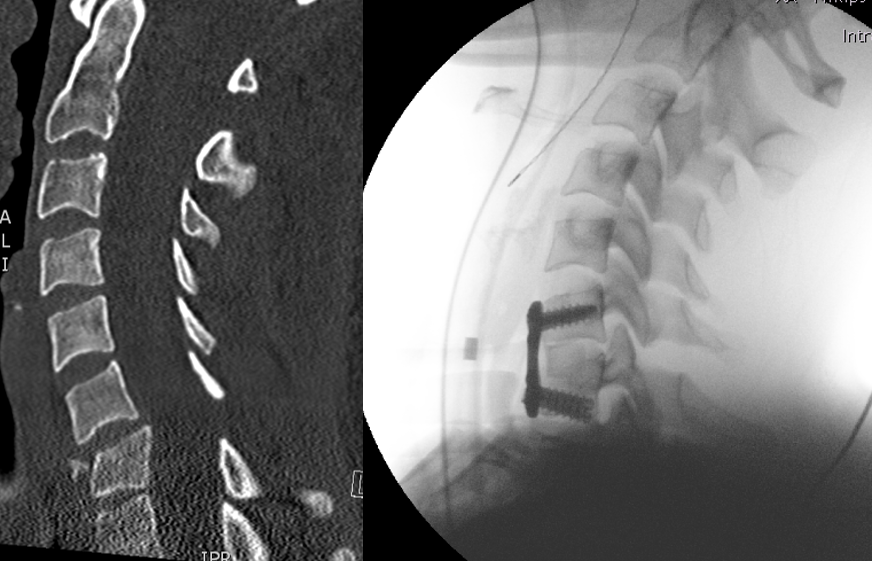
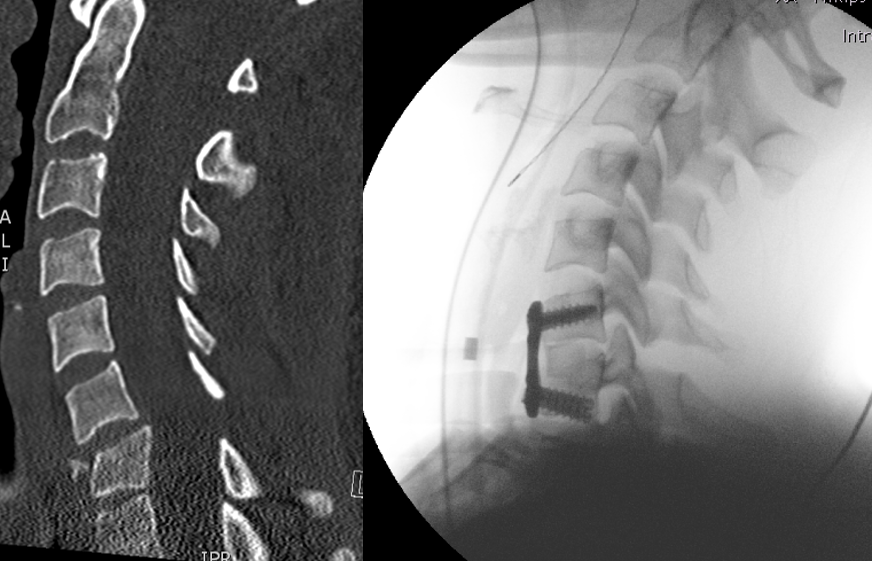
Illustration: Left: Computed tomography performed after an injury to the cervical spine, showing a misalignment and kink between the C6 and C7 cervical vertebrae. Right: Intraoperative X-ray image captured after realignment of the cervical spine and fixation with a plate and screw. Surgical access was obtained through the neck from the front.
Service spectrum
- Spinal column injuries, including neuroparalysis and paraplegia
- Osteoporotic vertebral fractures
- Spinal injuries in ankylosing spondylitis
- Metastatic tumorous disorders of the spine
- Inflammation in the spinal region
- Post-traumatic malalignments and wear and tear
- Interventional pain therapy for the spinal column and pelvis
Diagnostic and surgical equipment
- Surgical equipment
- Minimally invasive and navigated spinal surgery
- X-ray-permeable carbon fibre table top
- 3-D X-ray capability
- Kyphoplasty/vertebroplasty
- Endoscopic unit for minimally invasive vertebral body replacement
Diagnostic equipment
- Computed tomography (with contrast medium as appropriate)
- Core spin tomography
- SPECT/CT / SPECT/MRI
- Myelography
Dynamic roentgenological examinations
Second opinions
If you are already under treatment or would like to obtain a second opinion before undergoing a surgical procedure, we will be happy to assist you accordingly.
Spinal injuries (traumatology/trauma surgery)
Cervical spine
Injuries to the cervical spine range from simple sprains (whiplash trauma) to highly unstable injuries with potential or already existing neurological failures. Owing to the large diameter of the spinal cord in this region, neurological failures resulting in paralyses or sensory disorders are the most common result of injuries sustained in this spinal region.
When surgical intervention is in order, we offer all conventional procedures for surgical stabilisation. Vertebral body fractures in the cervical region of the spine are typically stabilised from the front (ventrally). Usually an access site is chosen on the side of the neck, and through it the unstable spinal column is stabilised with the use of plates, screws, and coated plastic implants. In certain cases it is necessary to introduce these items from behind (dorsally) or to combine procedures.
Thoracic spine
The thoracic spine is well protected by the bony rib cage. Injuries to the thoracic spine are therefore usually associated with accidents in which there is a transfer of force of great magnitude (traffic accidents or falls from great heights).
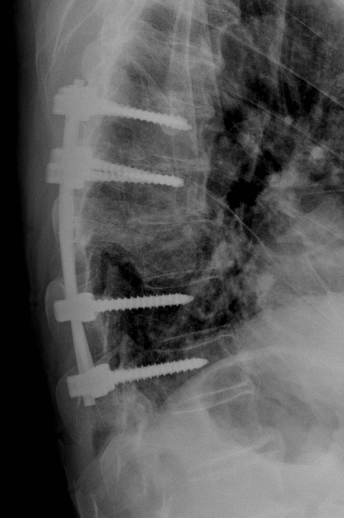
Typically the procedure for such injuries is stabilisation from behind (dorsally). A clamp is inserted to bridge the fractured vertebral bodies with the objective of decompressing them. Depending on the injury, this is accomplished by means of a minimally invasive procedure unless permanent fusion is indicated. Depending on the extent of the injury to the vertebral body or intervertebral disc, a vertebral body replacement from the front must be performed in the further course of treatment. As a rule, a “cage” (a vertebral body placeholder) or, more rarely, a bone chip taken from the iliac crest is used for this procedure. We routinely offer this operation by way of a minimally invasive open or “keyhole” technique whereby, depending on the technique employed, small pieces of a rib are removed and implanted in the region of the vertebral body. If the patient presents with painful vertebral body fractures that have no direct connection with the spinal canal, and particularly when the patient presents with osteoporotic bones, minimally invasive stabilisation procedures such as kyphoplasty (straightening of vertebrae and injection of bone cement) or vertebroplasty (injection of bone cement into vertebrae) also may be performed under certain conditions. As a rule, all of the techniques described above must be performed with cement reinforcement if the bones are osteoporotic. For these techniques we have at our disposal an extremely viscous and therefore reliable cement. As our objective is to progressively reduce the invasiveness of the necessary surgical procedures, we use a series of advanced techniques, examples of which include implants inserted in a minimally invasive manner into the vertebra from behind, an approach that enables us to avoid major operations from behind or the front.
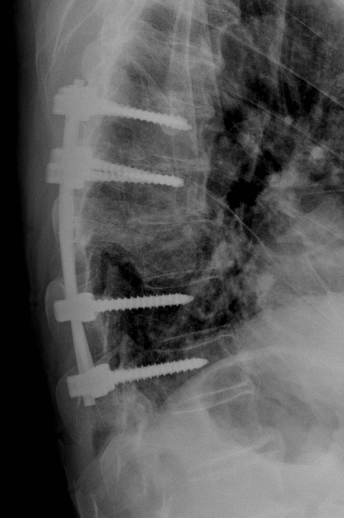
Illustration: X-ray image taken after treatment of a thoracic vertebral fracture with screws and rods.
Lumbar spine
Bony injuries to the spine occur most often in this region because the spinal column is exposed to the greatest biomechanical loads at the transition from the thoracic to the lumbar spine. Fortunately, the diameter of the spinal cord is smaller here than it is in the cervical and thoracic spinal regions, and for this reason, neurological failures occur relatively less often in this segment of the spinal column. Injuries to the lumbar spine, like those that occur in the thoracic spinal region, are usually stabilised initially from behind. Supplementary ventral stabilization procedures may be performed when necessary through the chest, applying the technique described above, or through a small incision in the trunk.

Illustration: Left: Computed tomography following a fracture of the L5 lumbar spine vertebra with constriction of the spinal canal by vertebral fragments. Right: Postoperative X-ray following combined stabilisation with screws from behind and rods from in front with removal of the broken vertebra and their replacement with a titanium placeholder. Room for the nerves was restored at the same time.
Osteoporotic vertebral fractures
The term ‘osteoporosis’ refers to bone atrophy in excess of that which normally occurs. There is a loss of bone mass as compared to age- and sex-specific norms. The remaining bone mass, however, remains normal in its composition.
The causes of osteoporosis are many. A basic distinction is made between primary osteoporosis, the cause of which is usually unknown, and secondary osteoporosis, which may arise as a result of various medical conditions.
Owing to a loss of bone mass, those segments of the skeletal system which, like the spinal column, are especially vulnerable to mechanical stresses, are subject to deformation and spontaneous fractures.
Typical symptoms include back pain, which radiological diagnostic procedures show to be associated with visible deformations of individual vertebrae (wedge-shaped, flat, or codfish vertebrae) and, in severe cases, spontaneous vertebral body fractures.
Depending on the symptoms and radiological findings, treatment may range from non-surgical treatment to minimally invasive stabilisation. Mechanical stabilisation must, however, be accompanied by medicinal therapy for the osteoporosis, which is applied on an interdisciplinary basis in consultation with our geriatricians.

Illustration: X-ray images captured after multiple osteoporotically fractured thoracic and lumbar vertebrae were cemented.
Spinal injuries in ankylosing spondylitis
Inflammatory process affecting the sacroiliac joint and the vertebral articulations. As in the case of rheumatism, a genetic component plays a key role in the development of this disorder. Men are more often affected by it than women, in whom the progression of the disorder is usually milder. The first symptoms usually appear between the second and fourth decades of life. Ossification of the connective tissue that surrounds the vertebrae results in progressive stiffening of the spinal column, which thereby loses its physiological elasticity and becomes highly susceptible to very unstable vertebral body fractures, especially in the cervical spinal region. Thus, for ankylosing spondylitis patients with vertebral body fractures, one should always aim for stable surgical treatment.
Tumorous disorders of the spine
As elsewhere in the body as a whole, for the spinal column a distinction is made between primary and secondary tumours and between benign and malignant tumours. Primary tumours are rare. It is considerably more often the case that one finds metastases from malignant tumours whose origin is located elsewhere in the body. One type of tumour that often manifests on the spinal column is the plasmacytoma. Metastases occur in carcinomas of the breast, prostate, and thyroid gland, among others.
Signs of a malignant process include:
- An unusual fracture location
- Localised pain on vibration or pressure
- Signs of a primary tumour
Apart from the vertebral fracture itself, symptoms associated with the spinal cord and with protruding nerve roots may occur. The treatment programme for tumorous disorders of the spinal column is highly complex and is planned in interdisciplinary tumour conferences. In addition to extracting and analysing tissue samples, we stabilise the affected vertebral body, free nerve structures that the tumour has constricted, and remove the tumour. We have also a procedure for controlled ablation of tumours with heat. This procedure can be used alone or as an adjunct to a stabilising procedure.
A condition in which tumour tissue presses upon the spinal cord is referred to as malignant myelon compression. This condition requires diagnostic clarification and treatment on an emergency basis. All patients who are referred with suspicion of malignant myelon compression are treated in conformity with a patient pathway that is developed jointly by all of the medical disciplines involved. For further details in respect of clinical indications of malignant myelon compression and referral and treatment of patients who present with it, please consult the information on the homepage of the Comprehensive Cancer Center Zürich.

Illustration: Left and centre: Computed tomography and magnetic resonance tomography of a cancer metastasis in the L3 lumbar vertebra. Right: Postoperative X-ray image taken after radio frequency ablation and stabilisation with radiolucent carbon fibre implants, which facilitate follow-up treatment of tumours.
Inflammation of the spine
Inflammation of the vertebrae (spondylitis) or intervertebral discs (spondylodiscitis) occurs usually as a consequence of blood poisoning, which often goes unnoticed, and manifests as back pain, fever and fatigue. In its early phase it must be differentiated from a malignant bone tumour.
Treatment of spondylitis or spondylodiscitis ranges from intravenous antibiotic therapy and rest to surgical removal and stabilisation, depending on the extent of the disorder.
Service spectrum
- Pelvic injuries
- Polytrauma
- Pelvic ring injuries
- Fractures of the hipbone socket (acetabulum)
- Femoral head fractures or fractures of the proximal femur
- Sports injuries in the pelvic region
- Treatment for the late effects of accidents
- Operations addressing cartilaginous tissue
- Implantation of artificial joints
- Geriatric pelvic fractures
- including minimally invasive procedures
- Sports injuries in the pelvic region
- Tumorous disorders in the pelvic region
- with an interdisciplinary approach
Special equipment
- Minimally invasive surgical technology
- Carbon fibre surgery table top
- Intraoperative 3-D imaging, including navigational equipment
Quality management
It goes without saying that our clinic participates in the Endoprosthesis Register of Switzerland. The objective is to further improve the already high quality of endoprosthetic treatment.