During a colonoscopy, the entire large intestine, the last few centimeters of the small intestine, the rectum and the anus are examined. In a survey of over 10,000 people, three quarters rated the screening colonoscopy as “good – acceptable”, 23 percent found it “somewhat unpleasant” or “unpleasant but bearable” and only one percent of respondents rated it as “very unpleasant”. On average, colonoscopy finds either adenomas (polyps) or, much more rarely, bowel cancer in 30 out of 100 people. The – objectively speaking very low – complication rates of colonoscopy are often overestimated.
What is a colonoscopy?
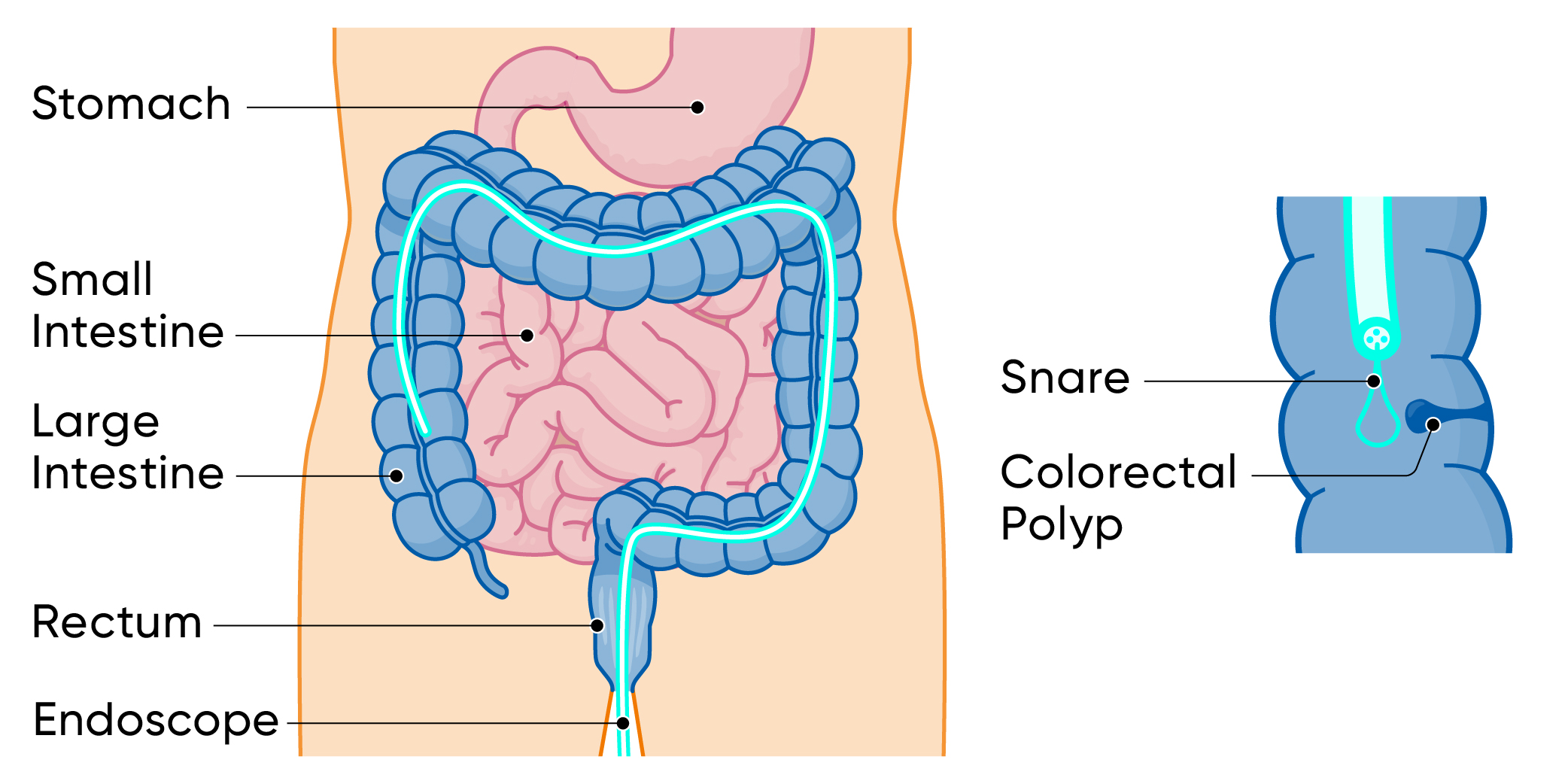
Colonoscopy is a highly developed medical examination method used for the early detection and diagnosis of bowel diseases such as bowel cancer. A gastroenterologist carefully inserts a flexible endoscope into the colon of a sedated (sleeping) patient in order to identify tissue changes, intestinal polyps or other abnormalities and, if necessary, to remove them directly before colon cancer can develop. This minimally invasive procedure enables a precise diagnosis and is a crucial step in preventive healthcare, especially for people over a certain age. The Cancer League recommends a colonoscopy for everyone aged 50 and over.
What are intestinal polyps?
Intestinal polyps are small, primarily benign growths that can develop in the mucous membrane of the large intestine. These polyps do not cause any symptoms, which is why they must be actively sought with a colonoscopy. Although most intestinal polyps are harmless, there is a risk that some of them can develop into malignant tumors over time. For this reason, early detection and removal of intestinal polyps is of crucial importance. Our highly qualified gastroenterologists specialize in identifying polyps in the colon and, if necessary, removing them safely during the colonoscopy. This preventive approach is an important protection against bowel cancer.
Colonoscopy preparation
What can I eat before a colonoscopy?
The gastroenterologist only has a clear view of the bowel if the preparation is good. Certain foods such as whole grain products, small seeds and fiber-rich foods should therefore be avoided in the days before the colonoscopy. These can otherwise block the channels of the colonoscope and obstruct the view.
The bowel must be emptied before the colonoscopy. Therefore, the evening before and the morning of the examination day, you drink a strong laxative with plenty of liquid (up to four liters in total, depending on the preparation). Purging in two “portions” instead of all at once improves the “cleanliness” of the bowel. The laxative no longer tastes as unpleasant as it used to. Mixed with a little lemon juice or syrup and well chilled, it tastes more pleasant.
Further helpful tips for preparation
- The quality of the colonoscopy can be significantly improved with good preparation. The aim is that only tea-colored, clear liquid comes out of the anus. In addition to the doctor’s instructions, there are helpful apps that remind you of the important points in the days leading up to the colonoscopy.
- If you are prone to constipation or are already being treated for constipation, please let us know or take your usual laxatives in addition to ensure good bowel evacuation. It is particularly annoying for the patient if the examination has to be repeated due to poor visibility.
- Let us take you to the colonoscopy and pick you up again. Or use public transportation. This is because if sleeping pills or sedatives are used, you will not be fit to drive afterwards.
- If you are taking blood thinners, you should clarify with your doctor beforehand whether (and when) you need to stop taking these medications before the colonoscopy. This is usually not necessary. Iron supplements should be stopped five days beforehand.
- Before your doctor wants to remove polyps with high-frequency current, it is important to inform him or her if you have a pacemaker, a defibrillator or a metal implant (for example an artificial hip joint).
How does a colonoscopy work?
You will receive a friendly welcome and be taken to your berth. There, the responsible MPA or nurse will review your documents, give you special “colonoscopy clothing” and place a venous line through which you will later be administered the short-acting sleeping pill “Propofol”. You will then be wheeled onto a couch in the examination room where you will be greeted by the responsible team. The doctor will also talk to you before the examination and final questions will be discussed and safety features queried. In 95% of cases, a colonoscopy is performed while the patient is asleep for reasons of comfort. Sedation is dispensed with on special request or, for example, in the case of very high obesity or severe lung disease, which can make sedation dangerous. As soon as you are asleep, the doctor will first examine the rectum with a finger; usually the rectum and anal canal are first examined in detail using a short proctoscope.
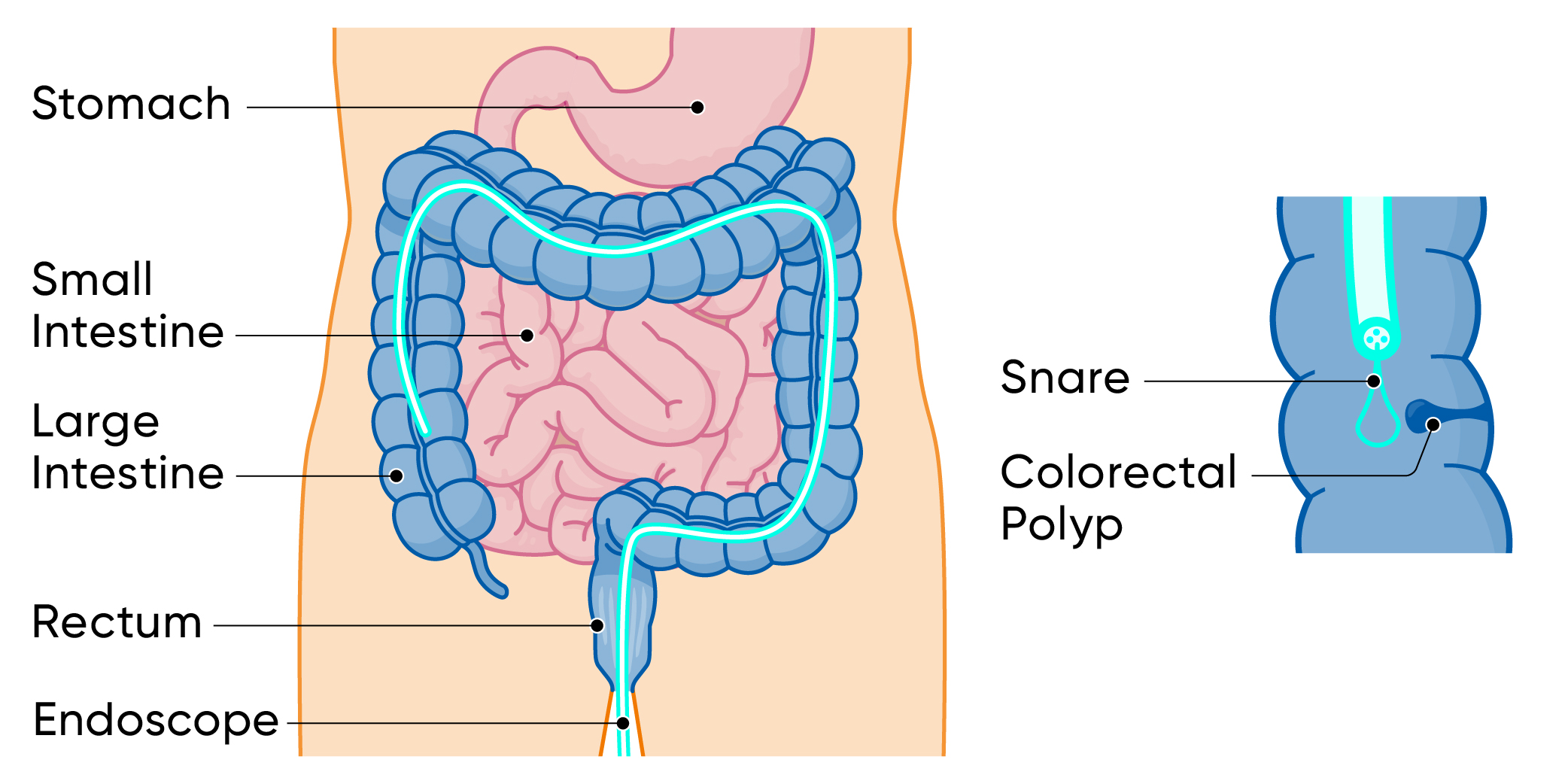
The actual colonoscopy is performed using an endoscope. This is a flexible tube about 1.5 meters long and around one centimeter thin. It contains a light source, a state-of-the-art computer chip that generates a video image and a working channel for thin instruments (forceps or snares) in a very small space. Devices are also attached to the tube to allow flushing of the instrument and insufflation, as well as suction of gas and fluid in the bowel. The images are transmitted to high-resolution monitors.
The doctor inserts the endoscope into the rectum from the anus and gently pushes the tip of the device through the large intestine until it reaches the end of the small intestine through the so-called ileocecal valve. It usually takes 10 to 15 minutes, depending on how tightly coiled the colon is, whether previous operations have made the abdomen more difficult to pass and whether, for example, in a very slim patient, the bowel gives way in the abdomen and is therefore more difficult to pass.
The doctor then slowly withdraws the endoscope and inspects the bowel from the inside. The intestine is inflated slightly with carbon dioxide so that it unfolds better. Carbon dioxide is better than air because it is immediately absorbed by the blood and then exhaled through the lungs. This avoids unpleasant bloating and pain after the endoscopy.
In an average of three to four out of ten people over the age of 50, the examiner finds one or more so-called adenomas (polyps). These are usually removed with the help of tiny forceps, a snare (with or without high-frequency current). He can take tissue samples from suspicious-looking areas of mucous membrane and use high-resolution images and special color filters to assess the bowel from the inside.
How long does the colonoscopy take?
All in all, the colonoscopy takes about 20 to 30 minutes. Only if the conditions are difficult and the bowel is very tortuous or if several polyps have to be removed can the examination take 50 or 60 minutes. If sleeping pills or tranquilizers have been used, the person tested will wake up quickly, but will not be fit to drive for the next twelve hours in accordance with the legal requirements.
Advantages and disadvantages
What are the advantages of colonoscopy?
It is the most reliable of all examination methods for the early detection of bowel cancer. If nothing abnormal is found, there is no need to undergo bowel cancer screening for ten years.
What are the disadvantages of colonoscopy?
The preparation for this is more complex than for the other common screening tests. Including preparation and debriefing, you lose about 1.4 working days. Adenomas or even small tumors can be overlooked during the examination. However, this is very rare with good preparation. Serious complications rarely occur during the examination.
What complications can occur during a colonoscopy?
Around 15 to 30 percent of people undergoing a colonoscopy experience abdominal pain, bloating or a feeling of pressure in the abdomen for a short time after the procedure because the bowel has been distended. Altered bowel movements or little blood loss also occur occasionally.
Overall, however, both colonoscopy and the removal of tissue or polyps are low-risk. Serious complications rarely occur. The figures vary from around one in 320 people to around one in 500 people examined. This usually affects older people with more comorbidities.
If complications occur, they are usually related to the removal of polyps. Less than one in 100 people examined bleed after polyp removal. Such bleeding can almost always be stopped immediately by endoscopy. Delayed bleeding after a few days is also possible, but rare.
In less than one in 1,000 cases, the screening colonoscopy results in a rupture of the bowel wall, which in the worst case can lead to surgery. This happens very rarely in a healthy intestine. If the colonoscopy was preceded by surgery on the bowel or neighboring organs, this complication occurs in around one in 300 people.
Rarely do sedatives and sleeping pills temporarily affect the heart or breathing.
Colorectal cancer screening: a colonoscopy is the best cancer prevention
Abnormal changes in the bowel can be detected better with a colonoscopy than with any other early detection method. With the regular screening colonoscopy…
- about eight out of ten colorectal cancers on the left side are prevented and about five out of ten on the right side
- colorectal cancer is detected with almost 100 percent certainty
- colorectal cancers in the entire colon are detected at an early stage, when the chances of recovery are still very good. More than eight out of ten colon tumors found by colonoscopy are still at this early stage
- the mortality rate from colorectal cancer is reduced by half
- 80 to 90 percent of adenomas (polyps) are found, which can usually be removed immediately during the examination. This eliminates the precursors of bowel cancer, as almost all bowel tumors develop from adenomas.
What does a colonoscopy cost?
Basic insurance pays for a screening colonoscopy every ten years for people between the ages of 50 and 69. If a diagnostic colonoscopy is necessary to clarify symptoms, the basic insurance always pays for the examination, minus the deductible and excess. Diagnostic colonoscopy is slightly more expensive than screening colonoscopy.
At what intervals should the colonoscopy be repeated?
If nothing abnormal is found during the screening or a maximum of two small, harmless polyps, it is usually sufficient to repeat the colonoscopy after ten years.
However, if there is an increased familial risk or if larger or more advanced polyps are found, they should be repeated earlier. In most cases, intervals of three to five years are sufficient. In individual cases, the gastroenterologist knows how best to proceed.
If symptoms suspicious of colorectal cancer occur in the interval between two screening colonoscopies, it may be advisable to perform the colonoscopy first. So-called “interval carcinomas” are rare, but cannot be ruled out, because adenomas (especially small ones) can be overlooked during colonoscopy.