Here at the USZ, you can have the scientifically based Stockholm3 blood test, which significantly improves the early detection of aggressive prostate cancer, carried out. It has been practiced in Sweden and Norway since 2017 and is now also available in other European countries.
Numerous scientific studies with a total of 75,000 participants have demonstrated the following advantages of the Stockholm3 test:
The Stockholm3 test
- is detecting more cases of aggressive prostate cancer,
- reduces the number of unnecessary prostate biopsies (removal of tissue from the prostate),
- detects aggressive cancer even in men with a low PSA (prostate-specific antigen).
Who can take the Stockholm3 test?
The test is suitable for men between the ages of 45 and 75 who have not yet had prostate cancer and whose PSA value is above 1.5 ng/ml.
Stockholm3 at the USZ
If you are interested in a Stockholm3 blood analysis, register now for a consultation. The Stockholm3 blood test is free of charge. The costs for the associated consultation and the PSA test are covered by the health insurance company.
How much does Stockholm3 cost?
The costs of the test are not yet covered by health insurance. Thanks to some subsidies, the test is free of charge for you. If you would like to bear the costs yourself or pay for another patient, we would be delighted – the funding will then last longer.
All consultations relating to the test and the PSA test, if necessary, are subject to a charge and are usually covered by health insurance.
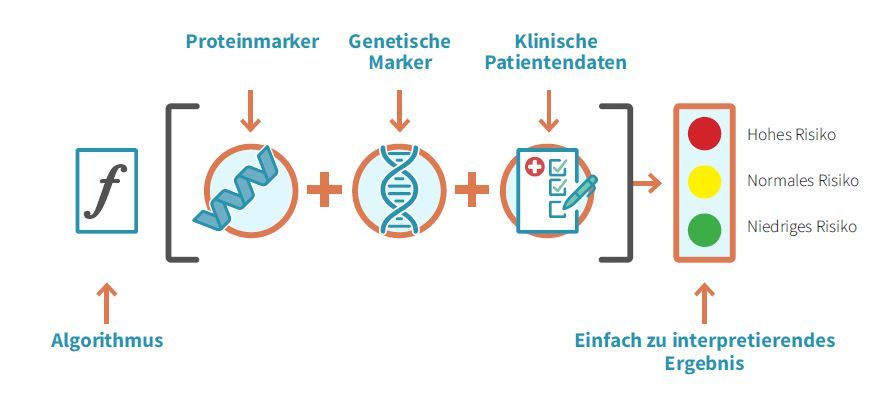
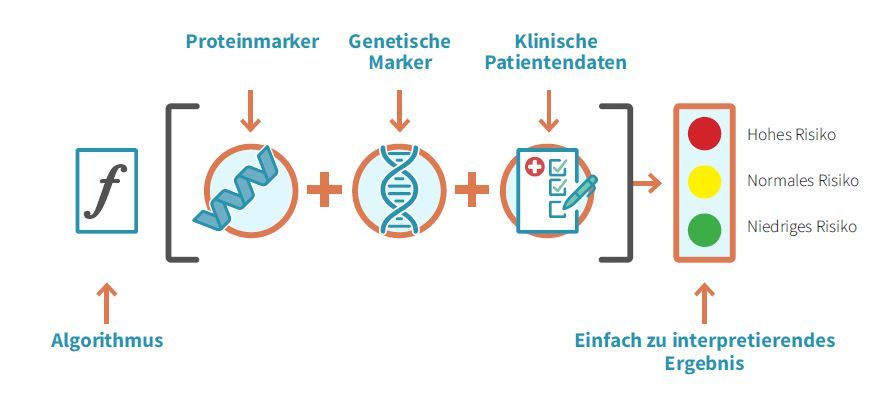
How does Stockholm3 work?
The Stockholm3 test is a blood test. This can be carried out from a PSA value of 1.5 ng/ml. Five different proteins and over 100 genetic biomarkers for the genetic risk profile are analyzed in the blood. The previous diagnostic standard, the PSA (prostate-specific antigen), is also determined. These laboratory values are combined with clinical data such as age, previous biopsies and family history in a risk score for the detection of aggressive prostate cancer at an early stage.
From a PSA value of 1.5 ng/ml, we can send blood samples from our patients to Sweden, where the laboratory analysis and bioinformatic evaluations are carried out anonymously. The treating urologist receives a clear treatment recommendation after the analysis. This may include, for example, that the risk of aggressive prostate cancer is low and that further screening in 1-6 years is sufficient. Or she recommends using further diagnostic procedures such as MRI (magnetic resonance imaging) or tissue removal from the prostate (biopsy) to clarify whether cancer could be present. All results are discussed with the patient and the next steps are decided.