For patients
In the obesity consultation, we discuss individual diet and exercise measures and evaluate drug and surgical therapies.
Surgery is advisable if all other conservative treatment options have not worked or if, after successful weight loss, there is always a sharp increase in weight, the so-called yo-yo effect.
Significant weight loss can be achieved through surgical intervention. The most common procedure in bariatric surgery is gastric bypass. For children and adolescents under the age of 18, surgery is an option if the BMIis over 35 kg/m2 and there is at least one serious concurrent illness. There is no upper age limit for bariatric surgery. However, operations over the age of 60 are generally associated with a higher risk.
The first step is to clarify whether you are generally suitable for bariatric surgery or whether surgical treatment is an option for you. If there are no objections to bariatric surgery, further clarification will follow.
The usual (minimum) clarifications include:
In some cases, the following examinations may also be necessary:
It can take between 2-4 months to carefully carry out the clarifications before an operation. This requires a little patience, but is time well and truly invested, helping you to reduce the risk of surgery as much as possible.
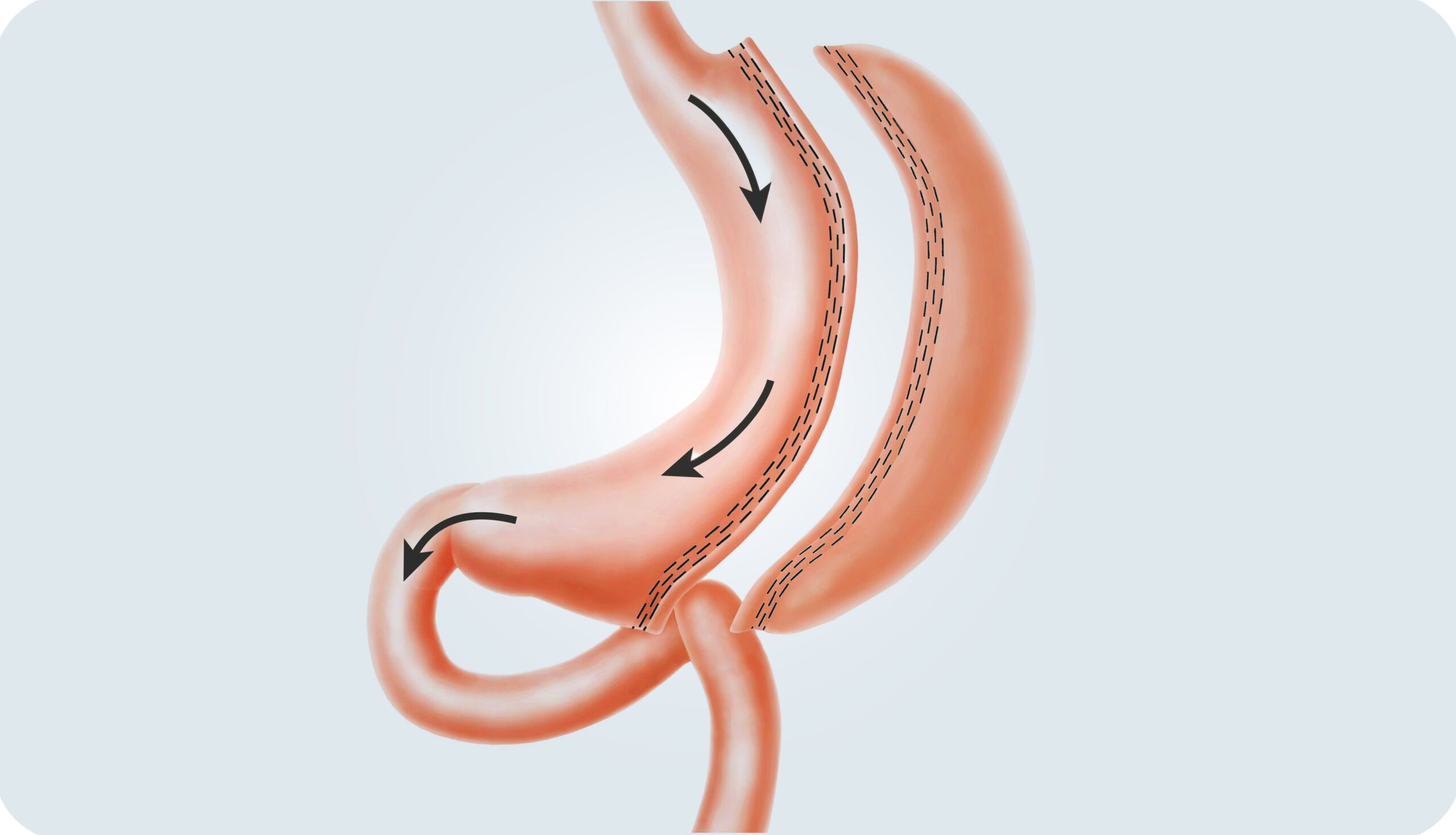
In this surgical method, part of the stomach is completely removed. What remains is an approx. two to three centimeter narrow tube (residual stomach), through which significantly less food can be absorbed. The feeling of satiety also sets in much faster. On the one hand, this results from the significant reduction in stomach volume. Secondly, the latest medical studies indicate that the production of the so-called hunger hormone (ghrelin), which is mainly produced in the stomach lining, is significantly reduced. Even though this surgical method is frequently used by us, it must be emphasized that no long-term results are yet available, as is the case with gastric bypass, for example. Nevertheless, our treatment successes show that with conscientious and professional aftercare and accompanying therapy, significant weight reduction is also possible in the long term. One advantage of the gastric sleeve is that the duration of the operation is usually shorter than with a gastric bypass or BPD (biliopancreatic diversion). This method is also often recommended as an initial procedure for extremely overweight people. After significant weight loss and stabilization of the general health situation, a second operation may be advisable. For example, conversion to a gastric bypass or the use of the BPD method.
Gastric bypass is one of the most widespread and established methods of achieving significant weight loss through surgery. Similar to a gastric sleeve, the stomach is significantly reduced in size so that much less food can be absorbed. Unlike the sleeve stomach, however, the residual stomach is not completely removed, but remains in the body and produces digestive juices. In addition, the small intestine is bypassed so that food and digestive juices can only mix later in the small intestine. As a result, some of the calories (fats and sugar) cannot be digested and leave the body in the stool. The body’s reduced ability to absorb sugar, fats and other food components promotes weight loss. At the same time, however, many nutrients, vitamins and trace elements are less easily absorbed by the body as a result of this surgical measure. This may make it necessary to take additional food supplements or mineral and vitamin preparations.
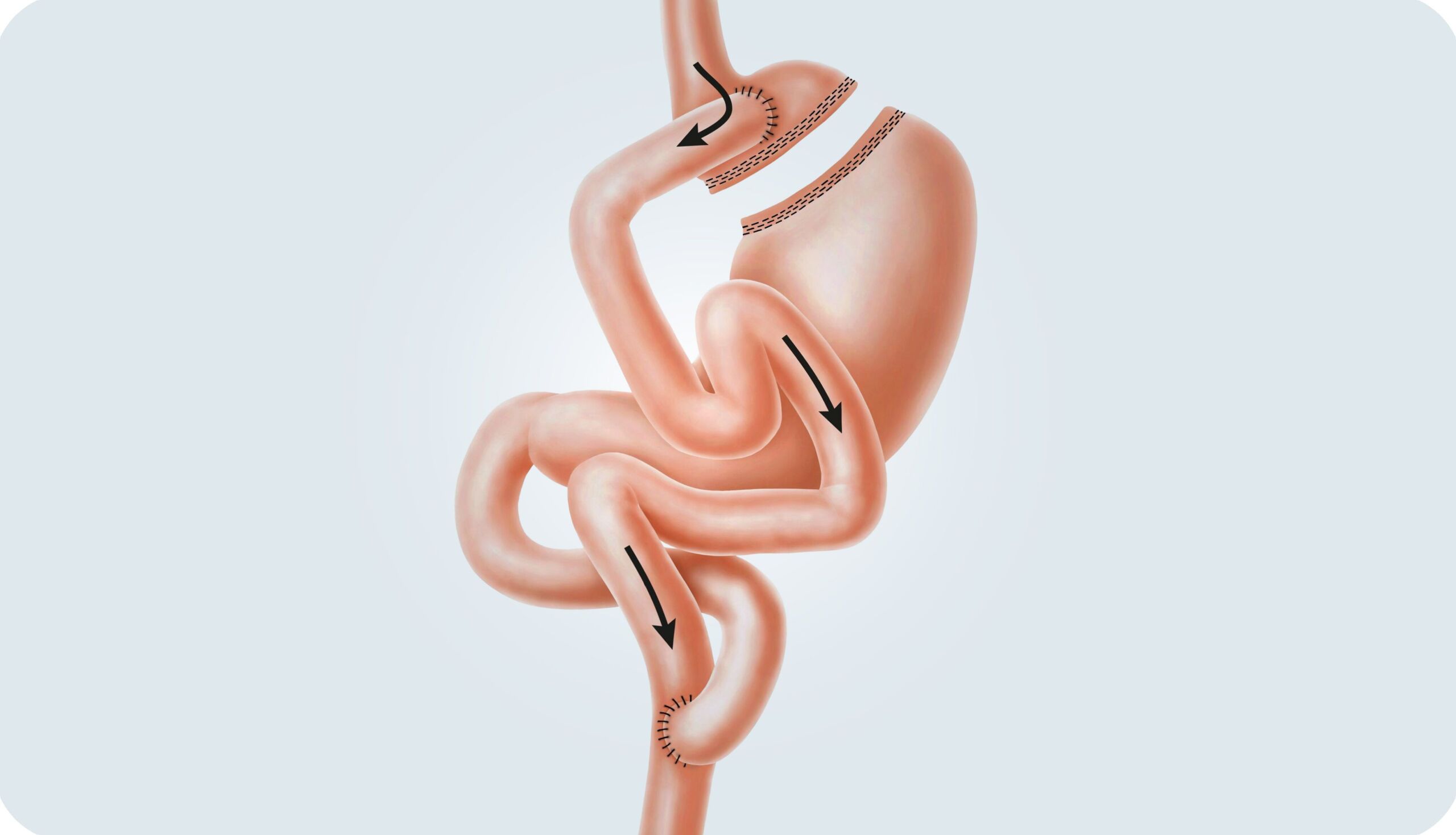
This procedure is only carried out by a few centers in Switzerland because this operation and the aftercare are particularly demanding. Even though this method is minimally invasive, i.e. it is carried out using the keyhole technique, many experts consider it to be the most effective method, but also the most invasive. In the broadest sense, biliopancreatic division corresponds to gastric bypass surgery, but in this case the remaining stomach is removed. In addition, the intestinal passage that connects the digestive juices with the food is only connected to the food-carrying intestine much later, so that the body can utilize fewer food components than with a gastric bypass. Internationally, this method is an established standard procedure and is often used for extremely overweight people with a BMI of well over 50. It is also possible to convert a gastric bypass or a gastric sleeve into a BPD if the previous methods have not brought the desired success or if weight regain occurs years later. Studies show that in addition to high weight loss, biliopancreatic division also produces the best results in the area of insulin regulation. Almost all type 2 diabetics who undergo such an operation are able to stop taking additional insulin preparations or other medications for this disease after the operation, or to greatly reduce the dosage.
Follow-up examinations are necessary. The weight progression is monitored and an optimal diet is discussed, which is adapted to the new situation after the operation and optimally supports the weight progression. It also ensures that no deficiencies occur. In addition, blood tests are carried out to determine whether the body is lacking certain nutrients such as vitamins or minerals, so that these can be supplemented with food if necessary.
In the first 1-2 years after the operation, the follow-up examinations usually take place one month after the operation, then every 3-6 months. If things go well, they can later be reduced to annual checks. However, our bariatric aftercare team is always available 24 hours a day to answer any questions or clarify any issues.
Large excess skin is often present after significant weight loss. These are usually located in the hip, breast, buttock or thigh area. This may require one or more surgical procedures to remove or tighten the skin tissue.
In the obesity consultation, we discuss individual diet and exercise measures and evaluate drug and surgical therapies.
Leading experts in the field of obesity from a wide range of disciplines work closely together to define a customized treatment pathway for your patients. We look forward to your assignment.
After a gastric bypass or gastric sleeve operation, a special diet is followed. On the first day after the operation, we start to build up your diet. One day of clear liquid, followed by 2 days of liquid food, 2 days of finely pureed food and then another 2-3 weeks of soft food. From about 3-4 weeks onwards, you can slowly switch to a normal diet.
In principle, the following applies:
Yes. Especially after gastric bypass surgery, you must continue with vitamin and mineral supplementation to avoid nutritional deficiencies. These deficiencies can be caused by reduced intake and difficulty absorbing nutrients after the procedure. There is also a risk of developing a disease caused by a long-term nutritional deficiency (e.g. osteoporosis). Most patients need a multivitamin preparation, calcium (approx. 1200 mg), iron for menstruating women (325 mg) and vitamin B12 (one injection per 3 months). Vitamins can be taken in tablet or liquid form. If you opt for a multivitamin tablet, take one in the form of a chewable tablet or a multivitamin for children. Do not take calcium and iron minerals together and try to avoid taking vitamins on an empty stomach.
In our experience, the majority of patients who have undergone gastric bypass or gastric sleeve surgery have reduced their excess weight by 50% after 6-9 months. The weight curve usually stabilizes after about 12-18 months.
The extent to which large excess skin flaps form depends on a person’s tissue type, the extent of weight loss and their age. If these skin flaps cause chronic irritation and infections, so-called fat apron operations can be covered by health insurance. The costs for this must be applied for from the health insurance company. The plastic surgeon will help with the application process. Health insurance companies usually make the assumption of costs dependent on the existence of health problems or a limited ability to work.
The side effects vary in their occurrence and extent and are difficult to predict. Some people report problems such as diarrhea, increased wind shedding and vomiting. Most side effects can be reduced by changing the composition of your diet. Malnutrition is rare with the current interventions, although vitamin/mineral supplementation is extremely important. All patients must take certain supplements for the rest of their lives, as the operation causes changes in the absorption of nutrients and reduced fluid intake.
This varies from person to person and depends on the procedure. Every postoperative complication understandably leads to a longer stay for the patient. On average, without complications after surgery, the stay for a laparascopic gastric bypass or sleeve gastrectomy is around 4-7 days. Patients can usually return to work 3-4 weeks after the operation.
The costs of surgery and the associated costs for anesthesia, hospitalization, medication, etc. are covered by health insurance if