A detailed diagnosis is important before any treatment decision is made. The examination results allow the doctor to determine the extent of the cancer and how aggressive it is. This is called staging. Based on the staging, the best possible treatment decision is made together with the patient. At the USZ, every bladder cancer case is discussed by several experts at an interdisciplinary tumor board in order to find the right treatment for each patient.
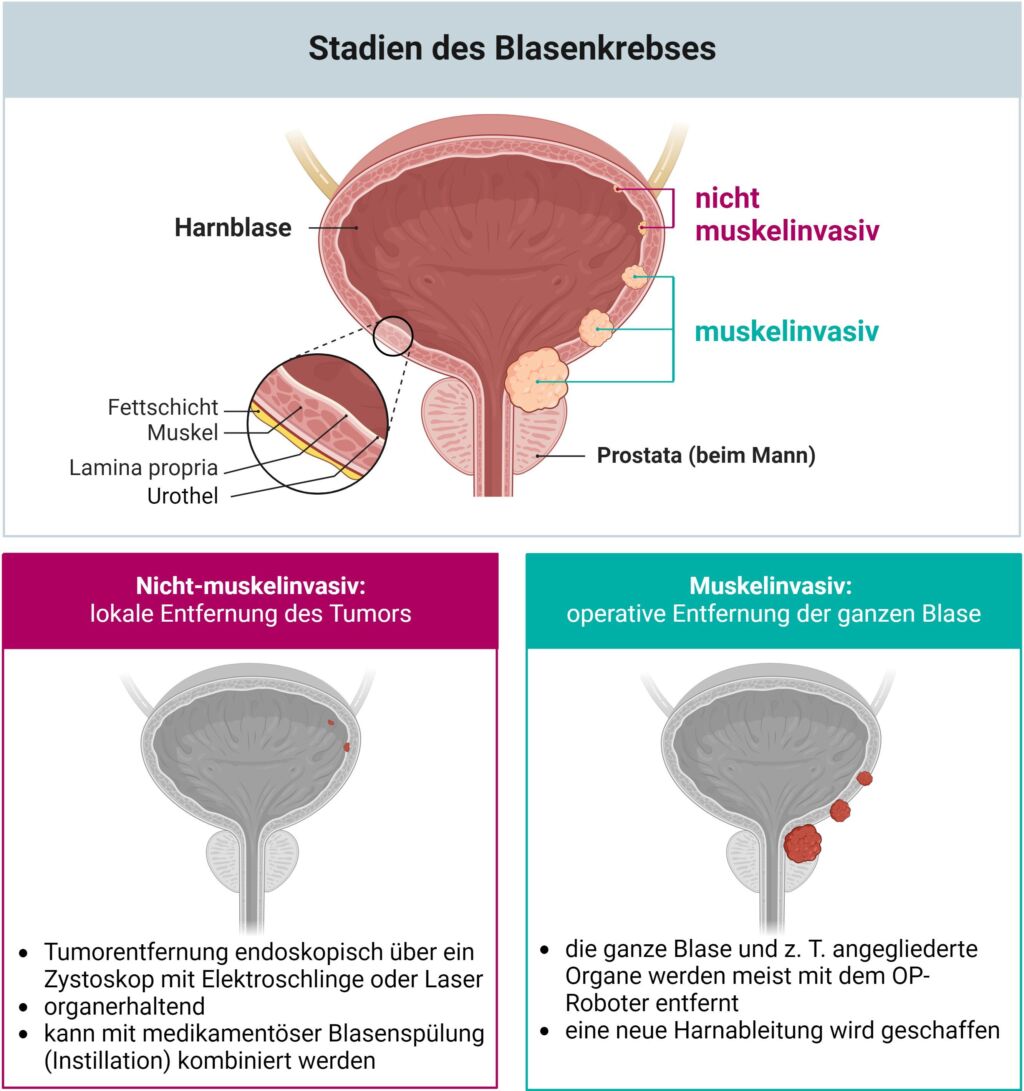
As a rough classification for possible surgical therapies, bladder cancer can be divided into non-muscle-invasive and muscle-invasive. Bladder cancer can only be cured if the tumor can be completely removed. If the cancer has already spread (metastasized), surgery is generally no longer performed.
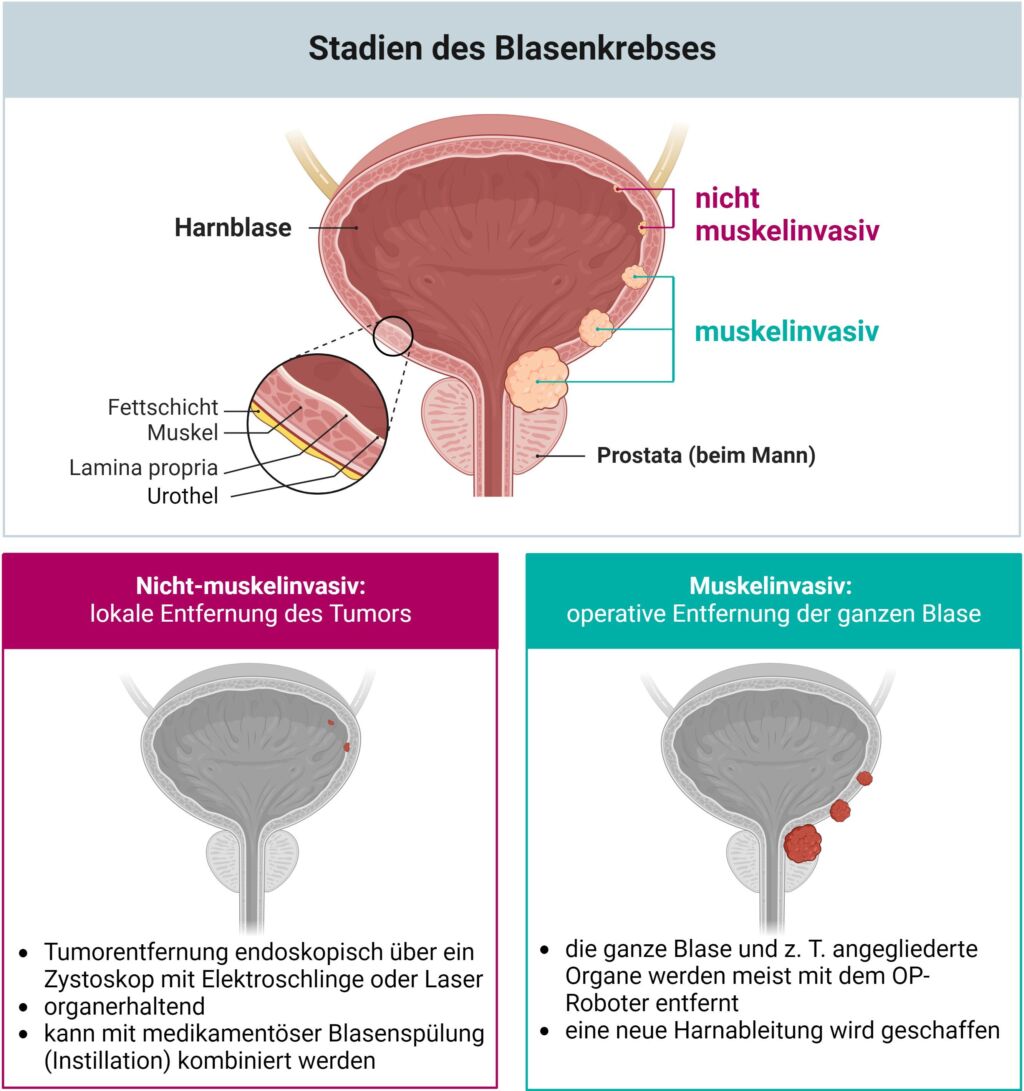
Non-muscle-invasive bladder cancer - organ-preserving local surgery
Superficial tumors can usually be operated on minimally invasively through the urethra. The procedure is called transurethral resection of the bladder tissue, abbreviated TUR-B, and is performed under partial or general anesthesia. An endoscopic instrument, the cystoscope, is used to insert a camera and a light source through the urethra. The doctor can use a monitor to assess the extent of the cancer and monitor the procedure. The tumor tissue is cut out of the bladder wall using an electric snare and removed via the urethra. The tumor tissue is used for histopathological examination. The Thulium fiber laser has recently been used at the USZ for tumor resection in addition to the electric snare (see info box).
After the operation, a bladder catheter is inserted and remains in place for 2-3 days. This prevents urine from accumulating in the bladder and gives the bladder wall time to heal. As a rule, this procedure is associated with a hospital stay of 2-3 days. After discharge, the patient is fit for work again, depending on the activity.
As the tumors can often recur over time (recurrence), close follow-up by means of cystoscopy is essential. In some cases, a secondary resection is also performed. Tissue is removed from the same areas again after a few weeks to ensure complete removal.
Removing bladder tumors with little bleeding using modern lasers
Since 2023, the Thulium fiber laser has been used in urology at the USZ alongside the electric snare for the gentle removal of non-muscle-invasive bladder tumors during cystoscopy.
The laser can be operated with very fine and flexible fibers and has a comparatively high output with low heat generation, which protects the surrounding tissue. The great advantage of this technique is that there is hardly any bleeding during tumor removal. This makes the method very gentle and suitable for many patients.
Local drug therapy (instillation)
In the case of non-muscle-invasive bladder cancer, a chemotherapy solution or a drug that activates the immune system (Bacillus Calmette-Guérin, BCG) can be flushed immediately after surgical removal of the tumor in order to destroy any remaining cancer cells. The medication is inserted through the catheter and remains in the bladder for up to two hours before it is emptied.
Muscle-invasive bladder cancer - Radical removal of the bladder (cystectomy)
If the cancer is already growing into the urinary bladder muscles (muscle invasive), there is a high risk that removal of the tumor via the urethra alone (TUR-B) will not remove all the cells and that the cancer will subsequently spread. For these reasons, the standard therapy for such a tumor stage is the complete removal of the bladder.
Even superficial but aggressive tumors occasionally have to be treated in this way. This is often treated with chemotherapy before the operation.
The removal of the bladder, called a cystectomy, is performed under general anesthesia. As a rule, the adjacent lymph nodes are also removed. Cystectomies at the University Hospital Zurich are performed entirely laparoscopically, i.e. minimally invasively, using the DaVinci surgical robot. This surgical technique is gentler than an open procedure and shortens the recovery time.
Read more about the operation with the robot
First, both ureters (connection to the kidney) are removed and the bladder is completely removed. In men, the prostate is always removed; in women, the uterus, ovaries and anterior vaginal wall can often be preserved, depending on the location of the tumor. After removal of the lymph nodes along the pelvic vessels, the urinary diversion is reconstructed.
Artificial urinary diversion
As a replacement for the removed bladder, there are various ways of draining urine from the body (internal and external drainage). One option is to construct a replacement bladder (neobladder) from a piece of small intestine, which is connected to the ureters. Urine is collected in the body in this new bladder. If the urethra is still present, it can be connected to the neobladder to expel the urine. This is controlled via the external sphincter muscles with training of the pelvic floor muscles. The bladder must be emptied actively every 4 hours (even at night) due to the lack of urge to urinate. A pouch (reservoir) can also be created as a variant of the neobladder. The urinary outlet is located on the outside of the abdominal wall and is emptied via a valve every 4 hours.
If a replacement bladder or pouch is not possible or not desired, a urostomy is constructed. The ureters are connected to a short piece of small intestine about 15-25 cm long, which serves as a flow channel. The open end of the piece of intestine is passed outwards through the abdominal wall. The urine leaks continuously and collects in a flat, waterproof bag that is placed around the urostomy. This bag must be emptied regularly and changed every two days.
This new situation of urinary diversion means a major change in everyday life and requires good training. We will not leave you alone with this. At the USZ, our ostomy counseling service is available to support you. Our ostomy consultants are also available to advise you in the run-up to the operation.
For stoma and continence advice
After the operation
After the operation, you will wear various probes and drainage tubes for about 14 days, depending on the type of urine drainage. An intravenous line is also set up for a few days to supply fluids and medication. Expect a hospital stay of at least 1-2 weeks. As a rule, you will be able to work again 10 – 12 weeks after the operation.
Treatment for metastatic bladder cancer
In the case of metastatic bladder cancer, systemic therapy (currently chemotherapy containing platinum, in some cases also immunotherapy alone) is the primary treatment. Surgery is rather rare at this stage.
Find out more about the risk factors, symptoms and diagnosis of bladder cancer on our website: Bladder cancer – USZ