In addition to the procedures that have been used for a long time (mammography, breast ultrasound), other interesting techniques (ultrasound elastography, tomosynthesis) have been added in recent years, which offer additional information for the assessment of pathologies or a higher level of detection accuracy in the detection of diseases. One method with very high accuracy is magnetic resonance mammography, which has been used increasingly in recent years for a wide range of different issues. Typical clinical questions in mammographic imaging are:
- the early detection of breast cancer (screening examination)
- the assessment of a lesion detected by palpation
- Breast pain (mastodynia)
- assessing the extent of a diagnosed breast cancer
- Aftercare after breast cancer
If you are unsure about the most suitable procedure, our doctors will be happy to advise you.
Diagnostic mammography
In addition to self-examination, mammography is the most important imaging examination method for the early detection (screening) of breast cancer. At the USZ we offer two different diagnostic methods:
World first: breast CT
The USZ is the first institute in the world to have a spiral computed tomography device for the female breast. This produces mammograms without the compression previously required. The patient therefore no longer needs to be afraid of the sometimes painful examination. The radiation dose is comparable to the previous devices. The images are three-dimensional and are evaluated according to the criteria of mammography, as both soft tissue structures and microcalcifications are visible. The appliance is not wheelchair accessible. The cost coverage of health insurance companies for a breast CT corresponds to conventional mammography with tomosynthesis. 
Conventional mammography
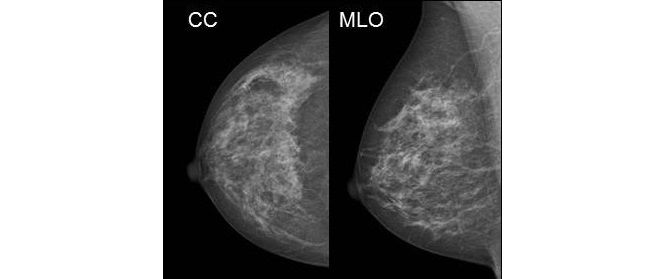
In the conventional method, the breast of the standing patient is fixed in the device between two Plexiglas plates. The images are taken from two directions: once from top to bottom (CC projection) and then from the center to the side (MLO projection). 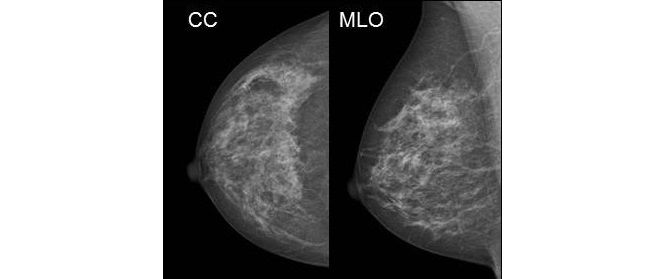 This pressure is necessary for the following reasons:
This pressure is necessary for the following reasons:
- The overlapping of glandular and connective tissue is reduced (the tissue is spread open)
- The contrast and image sharpness increase
- This improves the assessability of the mammogram, increases the diagnostic reliability of the radiologist and reduces the number of additional examinations
- Less radiation is needed
In dialog with the radiographer, the patient determines what degree of compression is tolerable for her.
Classification of breast density
The mammographic density of the glandular parenchyma is divided into densities between a (almost no more glandular parenchyma) and d (still very dense breast tissue) using the ACR classification. 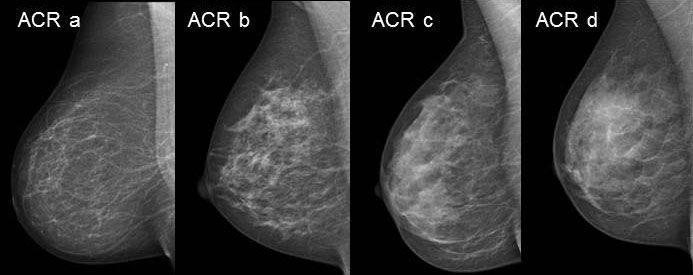 At ACR c and ACR d densities, the probability of detecting breast cancer is significantly reduced, so that a supplementary ultrasound examination is usually performed.
At ACR c and ACR d densities, the probability of detecting breast cancer is significantly reduced, so that a supplementary ultrasound examination is usually performed.
Breast sonography
Breast sonography (or breast ultrasound) is an important part of breast diagnostics, especially in younger women, in whom a mammogram can only be assessed to a limited extent due to the dense breast tissue. The ultrasound examination is based on the fact that mechanical waves (imperceptible and harmless) are introduced into the tissue using a so-called transducer. By reflecting the sound, information about the tissue density can be visualized. Due to the continuous development of the performance of ultrasound devices with better image quality, contrast and spatial resolution, ultrasound is able to find predominantly small invasive breast carcinomas. Ultrasound is also recommended as the preferred method for guiding percutaneous puncture and biopsy methods and for the preoperative localization of focal findings, not least due to its performance.
Indications
- Reliable diagnosis of the simple cyst
- Supplementary differential diagnosis of mammographic focal findings that are partially or completely overlaid by mammographically dense parenchymal structures
- Supplementary diagnostics for mammographically dense glandular bodies
- Clarification of palpation findings
- Complementary breast diagnostics for unclear mammography findings
Automatic 3D breast ultrasound
The Invenia ABUS breast cancer screening uses sound waves to create 3D images of the breast tissue. Unlike mammography, no ionizing radiation is used. The Institute of Diagnostic and Interventional Radiology is equipped with the first and so far only ABUS device in Switzerland. 
Indications
- Young women or women with dense breast tissue with an increased risk of developing breast cancer
- Follow-up checks in women with dense breast tissue who already have known benign lesions
- As an alternative to MRI for unclear findings
- Women with breast implants, to clarify the tightness
Breast magnetic resonance imaging
Since breast cancer tends to form new blood vessels (tumor neoangiogenesis), the contrast agent floods faster than in benign lesions. In addition, the contrast agent in the breast cancer is washed out more quickly (wash-out). Typical indications for a breast MRI are
- Preoperative local staging (local extent of findings, multifocality, multicentricity, exclusion of contralateral carcinoma)
- Early detection with a high-risk profile (BRCA 1/2)
- Monitoring under neoadjuvant therapy
- CUP syndrome (“cancer of unknown primary”)
- “Problem solver” for unclear findings in mammography/sonography
- Implants (question about rupture/capsular fibrosis)
Biopsy
If the imaging procedures show an abnormality, surgery is the only way to determine with certainty whether the change in the breast is malignant or benign. The surgeon is part of an interdisciplinary team and works closely with specialists from the fields of diagnostic imaging, pathology, radiotherapy, gynecological oncology and medical informatics.

 This pressure is necessary for the following reasons:
This pressure is necessary for the following reasons: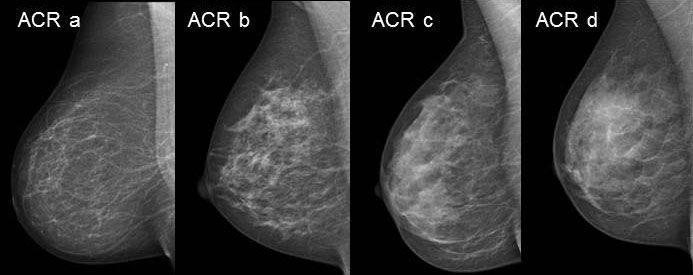 At ACR c and ACR d densities, the probability of detecting breast cancer is significantly reduced, so that a supplementary ultrasound examination is usually performed.
At ACR c and ACR d densities, the probability of detecting breast cancer is significantly reduced, so that a supplementary ultrasound examination is usually performed.

