Surgical therapy
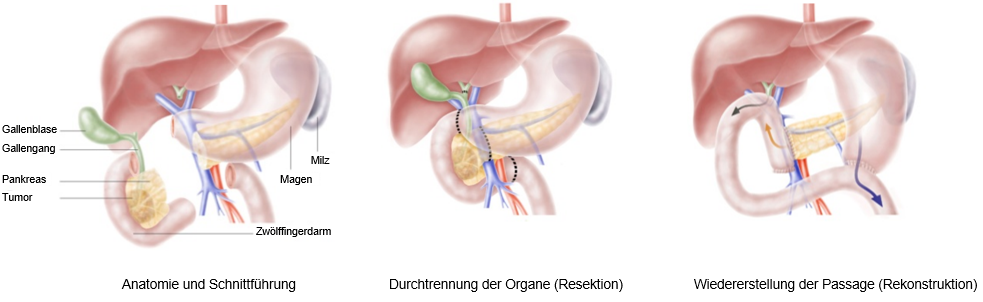
Complete removal of a pancreatic tumor is only possible through surgical treatment. It is the only way to achieve a complete cure (curative treatment). The preferred treatment for carcinomas located in the head of the pancreas is Kausch-Whipple surgery (figure).
In this procedure, the lower third of the stomach, the duodenum, the head of the pancreas with the carcinoma and surrounding lymph nodes, the gallbladder and the lower part of the common bile duct are removed in one piece (en bloc). In a frequently performed variation of the operation, the stomach remains completely intact.
A direct connection must always be established between the bile ducts at the liver portal and a loop of small intestine pulled upwards, as the natural drainage route into the duodenum cannot be maintained. The excretory duct of the pancreatic remnant (parts of the pancreatic body and the pancreatic tail) and the stomach must also be connected to this raised loop of small intestine.
The risk of leakage, particularly in the area where the small intestine and pancreas meet, is relatively high after surgery, especially if the pancreas is soft. However, only by means of this relatively extensive operation can a permanent cure be achieved at all in suitable cases.
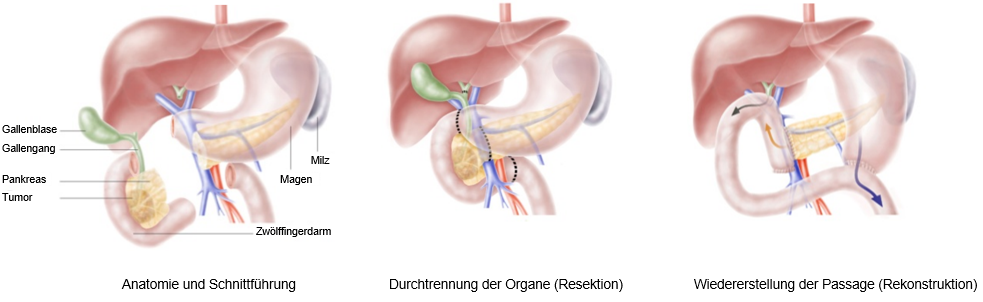
Operation according to Kausch Whipple
In the case of tumors in the tail and body of the pancreas, only the affected parts of the pancreas are removed. Often the spleen must also be removed in order to achieve sufficient radicality (complete tumor removal with lymph nodes).
Advances in surgical techniques and the high standard of intensive care medicine mean that these operations can now be performed at specialized centers with a good outcome and acceptable risk.
Maximum precision with robot-assisted pancreatic surgery (da Vinci®)
Robot-assisted pancreatic surgery (da Vinci) is a minimally invasive procedure. Like classic laparoscopy, it uses small access points through which the camera and instruments are inserted. With the da Vinci surgical system, the surgeon sits at a control console from which he or she has a full HD 3D view via the video system and guides the four arms of the robot. The strengths of the da Vinci surgical system lie in the exact representation of the anatomical structures and the extreme mobility of the robotic instruments, which make it possible to remove pancreatic tumors with high precision.
Robot-assisted surgery with the da Vinci surgical system (da Vinci XI) established itself in pancreatic surgery in 2019. Since then, patients undergoing oncological pancreatic surgery in particular have benefited from this state-of-the-art, minimally invasive procedure. The da Vinci surgical robot enables the surgeon to perform very complex operations (including robotic whipple surgery) despite the smallest incisions, where classic laparoscopy reaches its limits.
For the first time in Switzerland
Surgeons perform complex pancreatic cancer surgery with robots.
Nanoknife
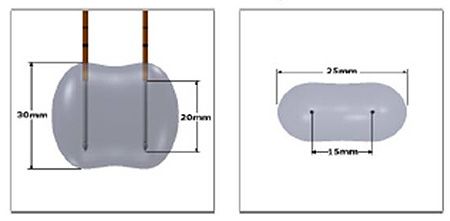
Nanoknife is a new local method for killing tumor tissue in which short bursts of alternating current are delivered through two or more electrodes placed precisely in parallel in the vicinity of the pancreatic tumor.
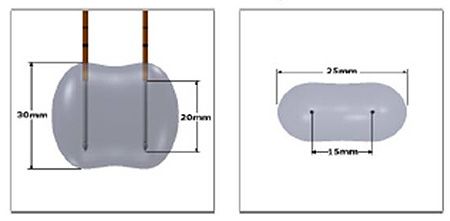
Visualization of nanoknife technology
Nanoknife kills the tumor tissue neither by heat nor by cold application, but by making the tissue avital through the flowing current. This method is also used in Zurich, particularly for non-resectable pancreatic tumors that are located near large blood vessels.
Chemotherapy
During chemotherapy, patients are given cytostatic drugs. Cytostatic drugs are plant-based or chemically produced substances that can destroy body cells or prevent or delay their proliferation. They work particularly well on rapidly dividing cells such as cancer cells.
Chemotherapy serves various purposes in the treatment of pancreatic cancer:
- Six-month follow-up treatment after a successful operation with the aim of healing; killing all cancer cells still present in the body.
- Reduction of a large pancreatic carcinoma to make it operable.
- Palliative therapy if the pancreatic cancer can no longer be cured; if other organs are affected, lymph nodes are affected, formation of distant metastases.
In the case of inoperable pancreatic cancer, chemotherapy can be combined with radiotherapy (radiochemotherapy).
Radiotherapy
If pancreatic cancer has been successfully operated on, radiotherapy is generally not necessary. If the pancreatic cancer cannot be operated on or cannot be completely removed, radiotherapy may be necessary to treat pancreatic cancer. Radiotherapy is also useful, for example, in the treatment of metastases in the brain and skeleton. Radiotherapy can destroy local cancer cells and reduce the symptoms caused by the metastases. Details on radiotherapy for pancreatic cancer can be found here.
Aftercare
After a successful pancreatic cancer operation, many cancer patients can breathe a sigh of relief. Nevertheless, follow-up examinations are very important in the further course. This is because the tumor can always recur. Follow-up examinations are carried out more frequently at the beginning and only every few months if the examinations are normal. Anyone who notices discomfort after the operation should have it checked out as soon as possible.
This is why regular follow-up examinations for pancreatic cancer are important:
- optimal treatment of possible consequences of the operation,
- proper adjustment of medication for type II diabetes mellitus,
- Drug replacement of the digestive enzymes no longer produced by the pancreas,
- Help for those affected by psychological or social problems.
Pancreatic cancer: using rehabilitation
Anyone who wants to recover well after cancer and regain their strength can take advantage of rehabilitation measures in a tumor aftercare clinic. Ask your health insurance company about rehabilitation options.

Certificate Publications