Risk factors
The risk of developing bowel cancer increases with age. On average, men fall ill at around 65, women at around 70. Only 10 % of colon cancers occur in patients under the age of 40. First-degree relatives (parents, siblings) of patients with colorectal cancer have an increased risk of also developing colorectal cancer. Patients with the rare genetic diseases FAP (familial adenomatous polyposis) or hereditary non-polyposis colorectal cancer syndrome (HNPCC) have a very high risk of bowel cancer. HNPCC is suspected when several first-degree relatives develop colorectal cancer at a relatively young age.
Symptoms
Symptoms of rectal cancer include bleeding from the anus, blood in the stool, stool irregularities (diarrhea alternating with constipation), pain or weight loss or the involuntary discharge of mucus or stool. If you have such symptoms, you should definitely consult your family doctor so that acolonoscopy can be carried out if necessary. With the help of this examination, such a tumor can be made visible or ruled out. These clarifications are all the more important if hemorrhoids or an anal fissure exist at the same time, which can cause similar symptoms and thus mask the symptoms of rectal cancer and delay the diagnosis.
Therapy
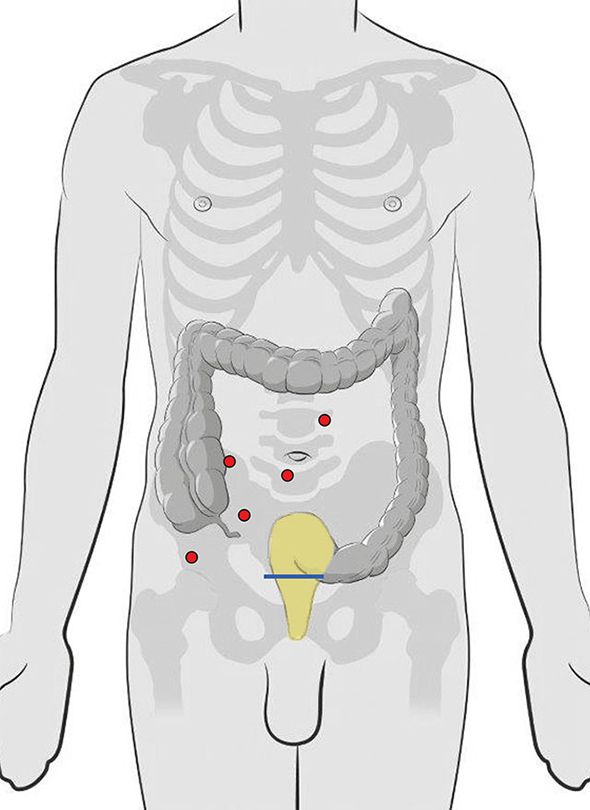
The malignant tumor in the rectum must be treated separately due to its location deep down in the pelvis and its proximity to the sphincter muscle. Cure can only be achieved by radical removal of the malignant tissue. If the malignant tumor is very close to the sphincter muscle or if it has already broken through the arm wall and grown into the surrounding fatty tissue, we recommend radiotherapy and, if necessary, chemotherapy before the operation. These measures can often shrink the tumor so that the sphincter muscle can be spared during the operation.
Surgical removal of the rectum is usually performed 8 to 12 weeks after pre-treatment (radiotherapy, possibly with chemotherapy). As a rule, the rectum is removed using a minimally invasive technique (laparoscopy or robot). A camera is inserted through a small incision and further instruments are inserted through additional skin incisions (0.5 to 1.5 cm). If the sphincter is not affected by tumor tissue, the rectum can be removed together with the adjacent fatty tissue immediately above it (deep anterior resection with total mesorectal excision) and removed via a small incision (7 to 10 cm) in the lower abdomen.
The surgical method with the robot is basically the same. The instruments are placed first (Figure 1), but the surgeon performs the operation at a console next to the patient (Figures 2 and 3). The robot can be used to work very precisely and gently. This is particularly advantageous in rectal surgery. A new connection (anastomosis) between the colon and anus is then created, whereby this new connection usually has to be protected with an upstream artificial bowel outlet (ileostomy).
Once the new colon connection has healed, the artificial bowel outlet can be closed after 6 to 8 weeks with a second small operation (ileostomy repositioning). If lymph glands are affected by tumor cells, the patient is recommended chemotherapy after the operation. If the sphincter muscle is permeated by tumor tissue, which is fortunately very rare, it cannot be preserved. Minimally invasive rectal surgery from the perineum is then supplemented with complete removal of the anus (abdominoperineal rectal amputation). The operation then ends with a permanent artificial anus. Here, too, it depends on the lymph node involvement whether additional chemotherapy is necessary. Surgical removal of the affected section of colon can lead to complete healing. Lymph gland offshoots or metastases in other organs (liver, lungs) are decisive for the prognosis.
Specialization in colorectal cancer surgery
The team of doctors led by Prof. Matthias Turina in the Clinic for Visceral and Transplant Surgery specializes in colorectal cancer surgery and works closely with specialists from other USZ clinics to ensure individual, high-quality patient care.
Surgical procedure - removal of the rectum
Rectum removal (laparoscopic or robotic) for malignant tumors
- Preparation: possibly radiotherapy or chemotherapy, small enema
- Anesthesia: General anesthesia
- Operation duration: 240 to 300 minutes
- Hospitalization: 7 to 10 days
- Incapacity to work: 3 to 4 weeks
- Follow-up treatment: possibly chemotherapy
- Follow-up checks: Tumor follow-up, check-ups after 3, 6, 12, 24, 36, 48 and 60 months
Open rectalectomy for malignant tumors
- Preparation: possibly radiotherapy or chemotherapy, small enema
- Anesthesia: General anesthesia
- Operation duration: 180 to 240 minutes
- Hospitalization: 10 to 14 days
- Incapacity to work: 4 to 6 weeks
- Follow-up treatment: possibly chemotherapy
- Follow-up checks: Tumor follow-up, check-ups after 3, 6, 12, 24, 36, 48 and 60 months
Complete removal of the rectum (including anus and sphincter)
- Preparation: possibly radiotherapy or chemotherapy, small enema
- Anesthesia: General anesthesia
- Operation duration: 180 to 240 minutes
- Hospitalization: 7 to 10 days
- Incapacity to work: 4 to 6 weeks
- Follow-up treatment: possibly chemotherapy
- Follow-up checks: Tumor follow-up, check-ups after 3, 6, 12, 24, 36, 48 and 60 months