Overview: What are hemorrhoids?
Hemorrhoids are vascular cushions located at the exit of the rectum near the anus. These erectile tissues are very well supplied with blood because they are supplied by a dense network of arteries and veins. Everyone has hemorrhoids, but they only become noticeable when they are pathologically enlarged. Doctors call this clinical picture hemorrhoidal disease or symptomatic hemorrhoids. In this case, the blood accumulates in the vascular cushions and can no longer flow away unhindered. This causes various symptoms, for example itching, burning, bleeding or oozing.
Hemorrhoids have an important task in the body: together with the internal and external sphincter, they seal the bowel and ensure that bowel emptying can be well controlled at all times. Sometimes these closure mechanisms also have to withstand greater stress, for example when great pressure is exerted on them when coughing, sneezing or lifting heavy loads.
Severity of enlarged hemorrhoids
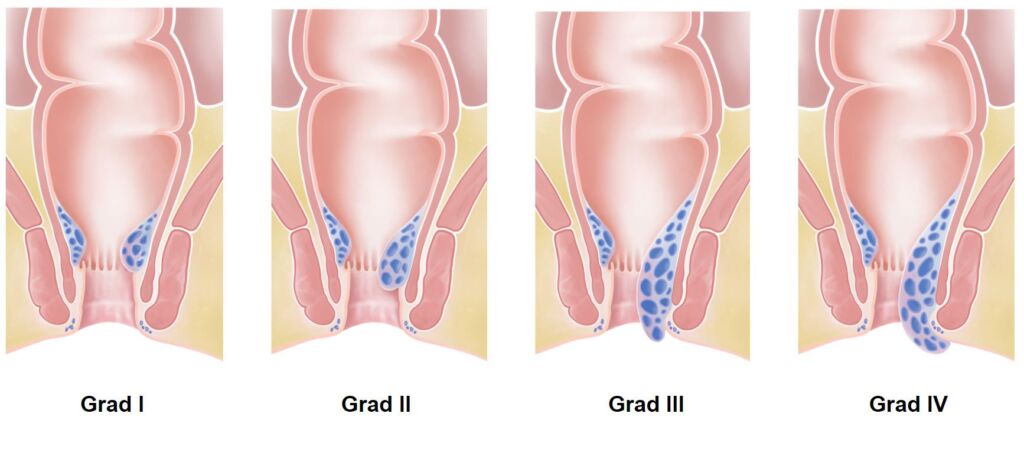
Depending on the size and severity of hemorrhoids, we divide them into different degrees of severity. There are grades one through four – from mild to severe hemorrhoidal disease.
- Grade 1: The hemorrhoids are enlarged but not visible from the outside. They usually do not yet cause any problems.
- Grade 2: The hemorrhoids are more enlarged. They may come out of the anus during bowel movements or sometimes during physical activity. However, they retreat back inside on their own.
- Grade 3: The hemorrhoids are enlarged to the point that they protrude from the anus during bowel movements and physical exertion. They will not slide back on their own, but you can push the erectile tissue back into place with the help of your fingers.
- Grade 4: The hemorrhoids are very enlarged. They emerge permanently from the anus and cannot be pushed back manually. So they are constantly visible from the outside. In most cases, a piece of the anal mucosa is also revealed. Doctors refer to this as anal prolapse.
Hemorrhoids – frequency and age
In industrialized nations, hemorrhoidal disease is one of the most common conditions. However, it is difficult to estimate exactly how many people suffer from this. This is because many people do not see a doctor for this reason, and the number of unreported cases is probably high. Medical professionals suspect that more than half of all adults over the age of 30 will develop problems with hemorrhoids during their lifetime.
Hemorrhoidal disease is most common between the ages of 45 and 65. Some studies conclude that men and women are affected about equally often. Other studies found that men are ahead in hemorrhoidal disease. During pregnancy there is often a temporary hemorrhoidal condition due to the hormone-induced weakness of the connective tissue.