Medication for ulcerative colitis
Drugs that dampen and contain inflammation are an important pillar in the treatment of ulcerative colitis. The following anti-inflammatory medications, for example, are used during an acute attack:
- Aminosalicylates: Active substances from this group intervene directly in the inflammatory process. Doctors mainly use the active ingredient mesalazine. The medication is also suitable for long-term treatment. Mesalazine prevents new relapses or reduces their frequency. The medicines are available in various dosage forms: as tablets, suppositories or foam and enemas for the rectum if the inflammation is located there. Possible side effects include headaches, diarrhea, hair loss or skin irritation.
- Probiotics: These contain health-promoting bacteria and can be an alternative to mesalazine – for example, if you cannot tolerate the active ingredient. The bacteria can prevent a further flare-up. Probiotics containing E. coli bacteria of the Nissle 1917 strain are recommended.
- Corticosteroids (“cortisone”): These are immunosuppressants that suppress the immune system. Doctors use it in acute flare-ups when aminosalicylates such as mesalazine have not shown sufficient success. However, drugs containing cortisone are not suitable for long-term treatment of ulcerative colitis due to the side effects. Prednisolone in tablet form is a commonly used active ingredient. Cortisone can also be administered as an infusion in higher doses. The active ingredient Budenoside helps if the inflammation is limited to the rectum. The medication is available as an enema, foam or suppository – it acts directly at the site of inflammation.
- Other immunosuppressants: These are used when mesalazine and cortisone have not produced a sufficient effect. Examples of alternative or additional active substances are azathioprine and 6-mercaptopurine. These immunosuppressants are suitable for treating an acute flare-up, but also for long-term therapy. They help to postpone a relapse for as long as possible. However, it takes a few months for the medication to take effect. So you need to be a little patient. Possible side effects: Headache, dizziness, inflammation of the liver and pancreas. Ciclosporin, methotrexate and tacrolimus are sometimes an option for very severe relapses. It also takes a few months for them to take effect.
- Antibodies (biologicals): These drugs intervene in the inflammatory metabolism and influence the immune system. Active substances for the treatment of ulcerative colitis include vedolizumab, infliximab, adalimumab or golimumab. The medication is available as an injection or infusion.
Please note the following: Medications that affect the immune system increase susceptibility to infections. Bacteria, viruses and fungi have an easier time of it. This increased susceptibility to infections can be a problem, especially for older people or those with other underlying illnesses. Always discuss the benefits and risks of all medications in detail with your doctor.
Surgery for ulcerative colitis
Ulcerative colitis can be cured with surgery. The standard procedure consists of the complete removal of the colon and rectum, the so-called total coloproctectomy. At the same time, a new reservoir for the stool is created with a small bowel loop and this is connected to the anus, the so-called ileo-pouch anal anastomosis (or IPAA). An artificial anus is then created to protect the newly created reservoir, which must be maintained for 8 to 12 weeks. After the healing phase, the artificial anus is closed again as part of a minor surgical procedure.
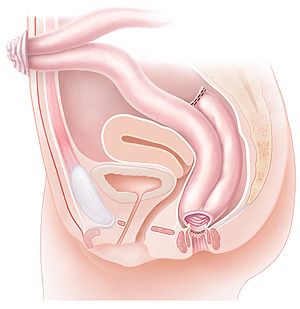 Total coloproctectomy and IPAA
Total coloproctectomy and IPAA
We perform this operation laparoscopically as standard, i.e. minimally invasive with the aid of keyhole surgery. The entire operation can be performed through three small (5 to 10 mm) and one slightly larger (4 to 5 cm) incision in the abdominal wall. This not only has cosmetic advantages. Patients recover much faster after surgery, have less pain, spend less time in hospital and can therefore return to work sooner.
Prognosis and course after the operation
After a total coloproctectomy and IPAA, there is full continence with a stool frequency of 5 to 6 bowel movements per day and 0-1 per night. Compared to bowel movements in ulcerative colitis, these are no longer explosive or painful and can be easily controlled. The quality of life is significantly better. Recent studies have also shown that the success rate of this operation over a longer period of time (20 years) is over 91% and that young women can also become pregnant and give birth normally after such an operation.
Nutrition as a therapy for ulcerative colitis
First of all, there is no special diet for ulcerative colitis. Make sure you eat a healthy, balanced and wholesome diet that meets your body’s nutritional requirements. Some tips on nutrition:
- During an acute attack, it is better to avoid foods that are difficult to digest and high in fiber. They would put even more strain on the intestines.
- A dairy-free diet suits some people
- Try out which foods you tolerate well and which you do not. Test this in phases in which you have no symptoms. Many patients do not like the following foods: flatulent fruit, vegetables and pulses, acidic citrus fruits (orange, grapefruit, pomelos, lemons), fruit juices, hot spices or alcohol. But they might be worth testing on a plate.
- Write down in a food diary which foods you have consumed and when. Keep a record of whether any discomfort has set in or whether the food has been good for you. Today, food diaries are also available in digital form, for example as a smartphone app. Otherwise, pen and paper will do.
- If your intestines are constricted, you should avoid foods with long fibers , such as asparagus or pineapple.
- If you are unsure about your diet: Consult a nutritionist (dietician, nutritionist).
Some people with ulcerative colitis suffer from deficiency symptoms. They lack important vitamins (e.g. vitamin D, vitamin B12) and minerals (e.g. zinc, iron). Then dietary supplements may be an option. However, you should not take them as a preventative measure, but only if a doctor has diagnosed a nutrient deficiency.
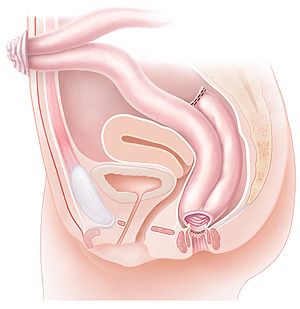 Total coloproctectomy and IPAA
Total coloproctectomy and IPAA