The most serious clinical manifestation of hypertrophic cardiomyopathy is sudden cardiac death, which occurs on average twice as often in these patients as in the normal population. Half of the patients with HCM have no or only very mild symptoms. Although hypertrophic cardiomyopathy cannot be cured, it can be treated well – with medication, interventional or surgical treatments.
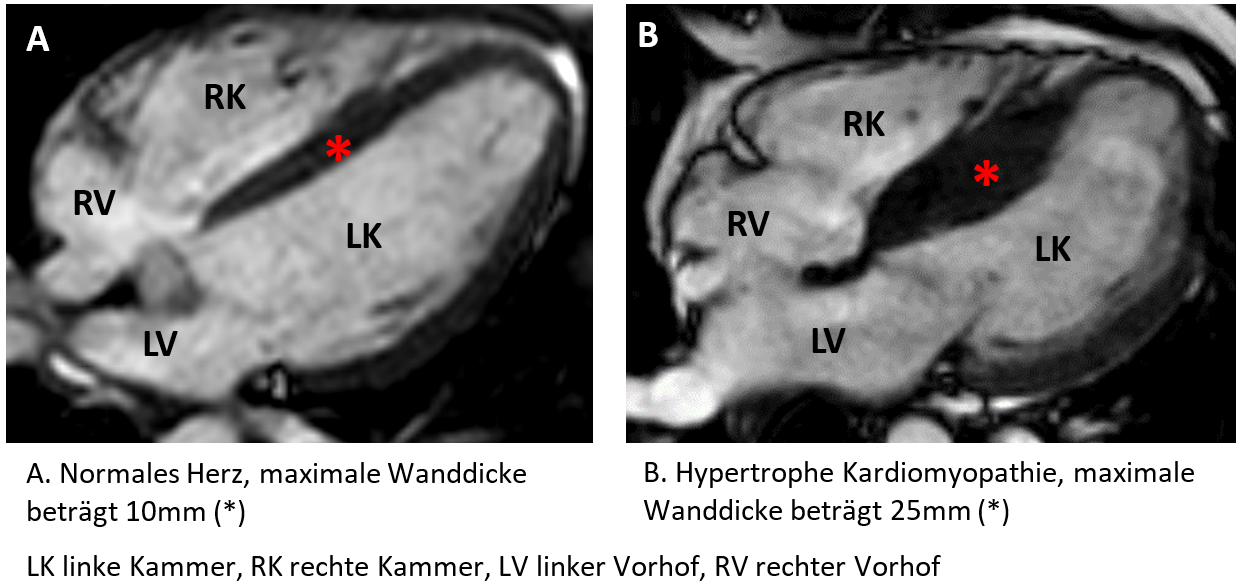
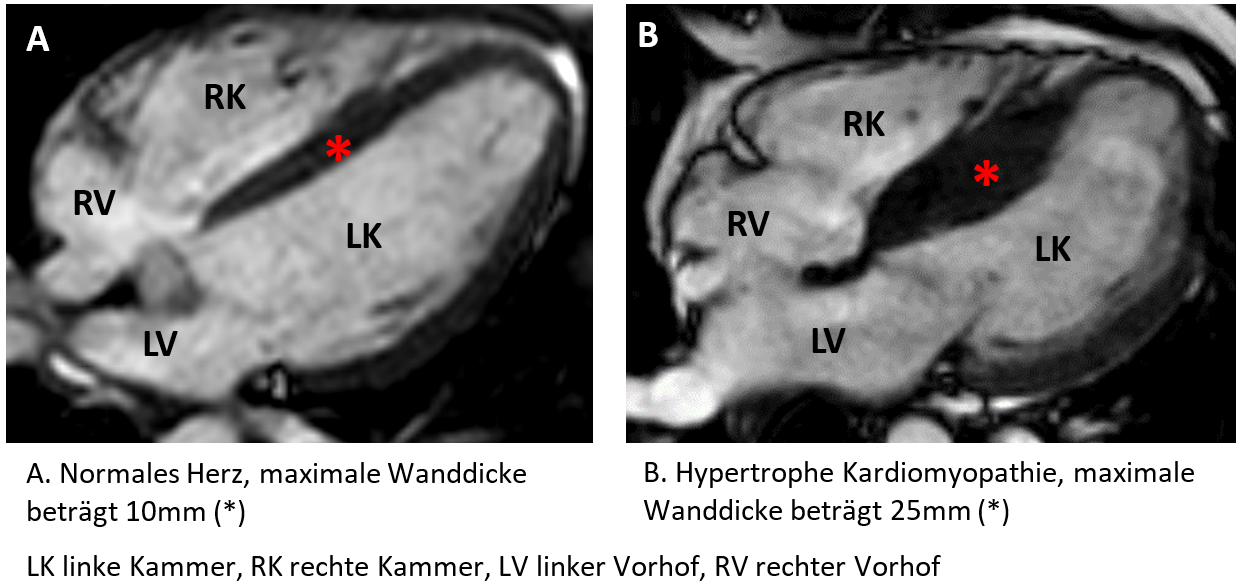
Hypertrophic cardiomyopathy is a mostly genetic heart disease in which the muscle cells in the heart wall become enlarged and the heart muscle (myocardium) thickens. In most cases, the left ventricle is affected, which can be up to two to four times thicker than a normal heart muscle.
Hypertrophic cardiomyopathy – frequency and age
In contrast to many other heart diseases, hypertrophic cardiomyopathy is rather rare: The incidence is 0.2% in the general population and can manifest itself at any age.
Hypertrophic cardiomyopathy - causes often lie in the genes
In many cases, hypertrophic cardiomyopathy is caused by defective genes. We estimate that around 40 to 60 percent of adolescents and adults with HCM have a genetic alteration in the cardiac sarcomere protein gene. This gene provides the building instructions for the sarcomeres, the smallest units of the muscles. If it is altered, the muscle cells and also the structure of the heart muscle deviate from normal. The muscle cells enlarge and the heart walls become thicker.
The mode of inheritance is autosomal dominant. This means that the mutation only has to be present on one of the two genes of the parents for a child to develop the disease (it receives each chromosome twice – once from the father, once from the mother). The probability that a child will inherit the “sick” gene is therefore 50 percent.
Even though hypertrophic cardiomyopathy is usually genetic and runs in families, different family members can develop the disease to very different degrees. The spectrum ranges from almost normal to a pronounced thickening.
Hypertrophic cardiomyopathy – other causes
There are also rarer genetic defects and non-genetic causes that lead to a thickening of the heart muscle and can present similarly to hypertrophic cardiomyopathy. In around 25 to 30 percent of patients with hypertrophic cardiomyopathy, unknown genes are altered (mutated). In around five to ten percent of adults, other diseases and factors are also involved:
- Congenital metabolic diseases, e.g. glycogen storage diseases, carnitine diseases, lysosomal storage diseases or Anderson Fabry disease
- Congenital diseases of the muscles and nerves (neuromuscular diseases), e.g. Friedreich’s ataxia
- Mitochondrial diseases, e.g. MELAS syndrome
- Malformation syndromes, e.g. Noonan or LEOPARD syndrome
- Amyloidosis
- Obesity
- Medication
As the correct diagnosis can have an impact on prognosis and treatment, we place great importance on the diagnostic process.
Hypertrophic cardiomyopathy - symptoms and expected complications
The symptoms of hypertrophic cardiomyopathy depend on how severe the disease is. Some people only experience mild symptoms, while hypertrophic cardiomyopathy causes more pronounced symptoms in others. These can have a significant impact on everyday life, enjoyment of life and quality of life.
Patients with hypertrophic cardiomyopathy can develop various complications during the course of the disease.
- Narrowing of the outflow tract of the left ventricle (obstructive form), which leads to a reduction in the volume of blood available to the body for its functions. Clinically, this usually manifests itself in a decrease in physical performance. Approximately 70% of patients can develop such a narrowing of the outflow tract.
- Stiff left ventricle (‘diastolic dysfunction’): the thickening of the heart muscle means that the left ventricle is rather stiff and cannot relax as well during the filling phase, when the heart absorbs blood from the systemic circulation. This increases the pressure in the heart, which can be accompanied by shortness of breath on the one hand and a feeling of pressure in the chest on the other.
- Heart failure: a small number of patients (5-10%) may develop a decrease in pumping function during the course of the disease, which then leads to heart failure. This can be accompanied by water retention in the legs and lungs (shortness of breath, coughing when lying down) or generally by tiredness and a decrease in performance.
- Atrial fibrillation: this is an arrhythmia that originates in the left atrium and is usually accompanied by a rapid, irregular pulse. This arrhythmia is not life-threatening, but usually leads to clear symptoms. It is extremely important to start blood thinning so that no clots can form in the heart, which in the worst case could cause a stroke. Approximately one third of patients with hypertrophic cardiomyopathy develop atrial fibrillation during the course of the disease, which usually only lasts for a short time at the beginning but can remain permanent in extreme cases.
- Sudden cardiac death: this is the most serious complication, but fortunately it is rare. The event rate in patients with hypertrophic cardiomyopathy is 0.6% per year, compared to 0.3% per year in the normal population. This arrhythmia does not announce itself in advance and can occur from a state of absolute well-being, leading to circulatory collapse and death if first aid is not provided quickly
Hypertrophic cardiomyopathy: treatment options and behavioral measures
Doctors from different specialist disciplines are involved in the treatment of hypertrophic cardiomyopathy. The clinical cardiologist, who sees the patient in the consultation and then, depending on the main problem, seeks interdisciplinary treatment and care with the relevant specialists from the other disciplines, is central. Hypertrophic cardiomyopathy cannot be cured. However, we can treat the symptoms well and reduce the risk of complications such as sudden cardiac death.
The following treatment options are available:
- Narrowing of the outflow tract of the left ventricle: this is primarily done with medication to relieve the heart and facilitate the flow of blood from the heart into the circulatory system. Examples are beta-blockers (bisoprolol, metoprolol, etc.) or calcium antagonists (verapamil, diltiazem). If the medication is not sufficient, more invasive methods are used with the aim of thinning the thickened muscle tissue in the outflow tract of the left ventricle so that the blood can flow freely again. This includes septal alcohol ablation, in which the cardiac catheter specialist injects alcohol into the small arterial blood vessels that supply the cardiac septum, thereby obliterating the thickened tissue. Another option is surgical myectomy, in which the heart surgeon removes part of the thickened heart muscle from the outflow tract with a scalpel.
- Stiff left ventricle (‘diastolic dysfunction’): Medication is primarily used here, including beta blockers or calcium antagonists.
- Cardiac insufficiency: Medication is used here that is also used for other forms of cardiac insufficiency, with the aim of relieving the heart and stabilizing the pumping function for as long as possible. In extreme cases, treatment for these forms can go as far as a heart transplant, but this is very, very rare in patients with hypertrophic cardiomyopathy.
- Atrial fibrillation: here we try to bring the heart back into normal rhythm either by medication or electrically by cardioversion (application of electricity during short sleep). Subsequently, rhythm-stabilizing medication is usually administered as long-term therapy. It is of the utmost importance to start permanent blood thinning to prevent the formation of blood clots in the heart and to prevent strokes. If the atrial fibrillation episodes become more frequent, catheter-controlled obliteration of the arrhythmia can also be discussed.
- Sudden cardiac death: The risk of sudden cardiac death is reassessed for each patient at each consultation. If the risk is considered high, we recommend the implantation of an implantable cardioverter defibrillator (ICD). This cannot prevent the occurrence of the arrhythmia and does not reduce the symptoms. But it acts as a guardian angel and, if the potentially fatal arrhythmia occurs, delivers an electric shock from within to stop the arrhythmia. Patients are usually unaware of this because they have often lost consciousness at this point.
Sports recommendations
We recommend moderate endurance sports with a warm-up and warm-down phase. Running, jogging, cycling, swimming, etc. are ideal. What patients with hypertrophic cardiomyopathy do not tolerate well are sports that involve sprints (e.g. squash, badminton, singles tennis). We also advise against intensive strength training; at least 15-18 repetitions should be possible. We also advise against competitive sports. For very athletic patients, we also offer an interdisciplinary consultation with our sports cardiologists.- General behavioral measures: in principle, there is nothing that affected patients can do to prevent the development of the disease. However, by stopping smoking and moderate alcohol consumption, patients can ensure that their heart is not additionally damaged, e.g. by a heart attack, which is facilitated by smoking. We also strongly advise against the use of substances such as cocaine, LSD, etc., as these can trigger arrhythmias.
Course and prognosis of hypertrophic cardiomyopathy
The course and prognosis of hypertrophic cardiomyopathy naturally vary from patient to patient and cannot be predicted in detail for each individual patient. As described above, a variety of complications can occur, which can have lasting effects on the individual patient.
It is fair to say, however, that life expectancy has become similar to that of the normal population in recent decades thanks to the use of the above-mentioned treatment options, including defibrillators, invasive interventions and even heart transplants in rare cases. As a result, hypertrophic cardiomyopathy is now an incurable but easily treatable heart muscle disease.
The initial evaluation is usually carried out during an outpatient appointment in our special consultation for hypertrophic cardiomyopathies. A detailed medical history (anamnesis) of the patient and their family is essential. It is therefore advantageous if patients are well informed and, if necessary, bring documents with them to the consultation. In addition to the physical examination, we routinely carry out a cardiac waveform(ECG), a blood test, a stress test and an ultrasound of the heart (transthoracic echocardiography). We also prescribe patients a long-term ECG (24-48h) and arrange for a magnetic resonance imaging (MRI) of the heart if this has never been carried out before.
These are many examinations, but they allow us to narrow down the diagnosis – is it really hypertrophic cardiomyopathy or do we have to consider other causes of cardiomyopathy? – On the other hand, they allow us to assess the severity of the disease and, in particular, the risk of arrhythmia.
Based on these examinations, we can make recommendations for any further investigations that we may need, for example, if we suspect a metabolic disorder (e.g. bone scintigraphy if amyloidosis is suspected). In addition, these examinations enable us to suggest optimal drug therapies and to assess which patients have a significantly increased risk of sudden cardiac death and would therefore benefit from the implantation of a defibrillator.
An initial evaluation including cardiac MRI takes about half a day with all examinations, without cardiac MRI about three hours.
Further clarifications include the possibility of a genetic clarification as part of our cardiogenetic consultation, as hypertrophic cardiomyopathy is usually a genetic disease. In this context, it is important to note that clinical family screening with ECG and ultrasound of the heart is highly recommended for all first-degree relatives. The aim of these screening examinations is to be able to detect the disease at an early stage in order to ideally prevent sudden cardiac death as the first manifestation of the disease. If a disease-causing gene mutation is found in the family during genetic testing, the family members can of course also be tested for this gene mutation.
For stable patients, we recommend annual follow-up checks with clinical assessment, ECG, blood test, ultrasound of the heart, stress test and long-term ECG in order to be able to recognize and treat any complications at an early stage. We repeat the heart MRI every three to five years, as this gives us valuable additional information in addition to the ultrasound.
For patients who suffer from a relevant narrowing of the outflow tract of the left ventricle despite extensive drug therapy, we naturally offer the evaluation and implementation of invasive therapy options such as septal alcohol ablation and surgical myectomy.
Self-help groups
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group is available from Selbsthilfe Zürich. Self-Help Zurich and the University Hospital Zurich are cooperation partners in the national project “Health literacy thanks to self-help-friendly hospitals”.