What is a melanoma
Melanoma, also known as malignant melanoma, is the most dangerous form of skin cancer. It develops from the pigment-producing cells of the skin, the melanocytes. These produce the pigment melanin and are therefore responsible for tanning the skin. In melanoma, the melanocytes degenerate and multiply uncontrollably. In addition to melanoma of the skin, in rare cases melanoma can also develop on the mucous membranes inside the body or in the eye.
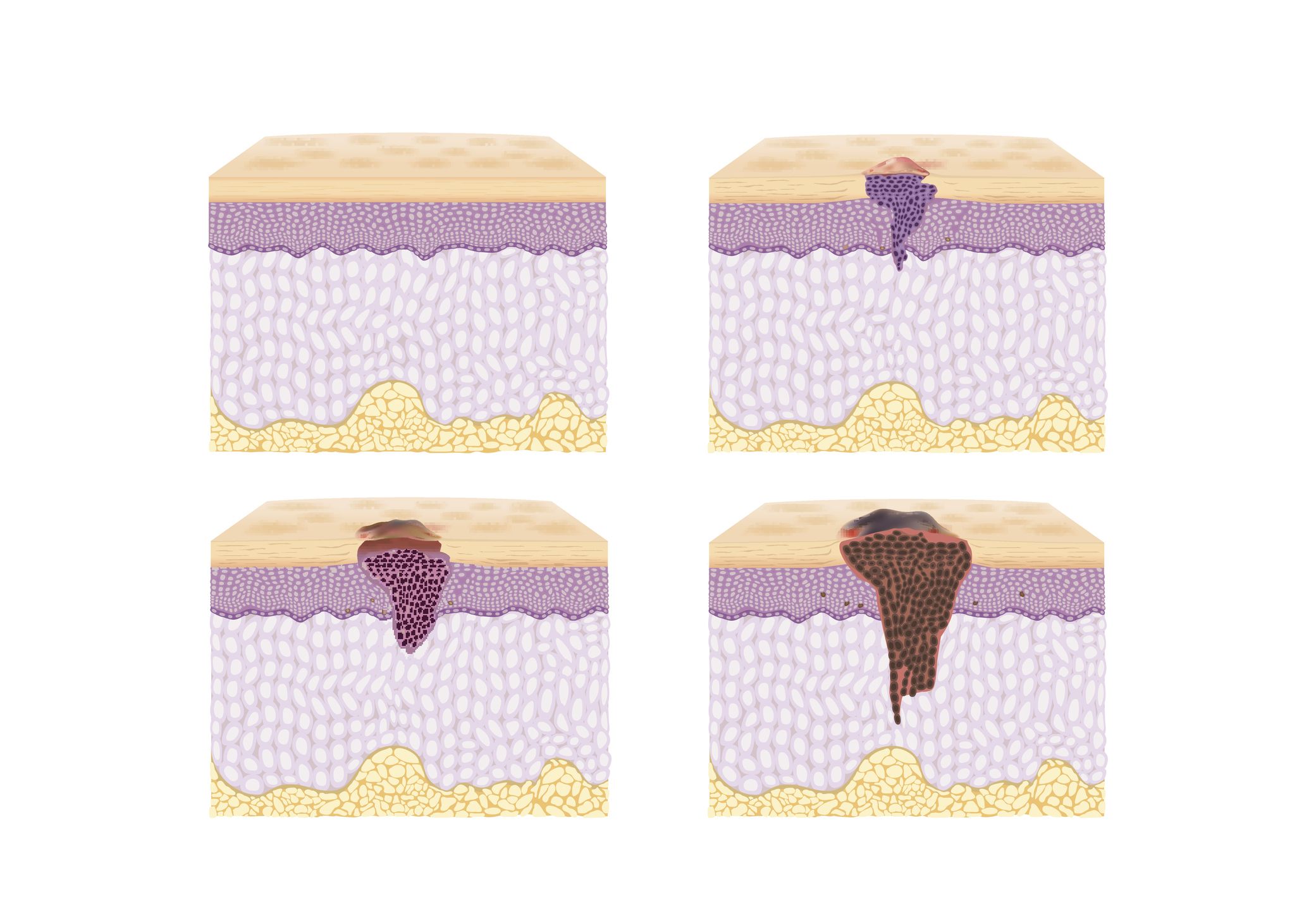
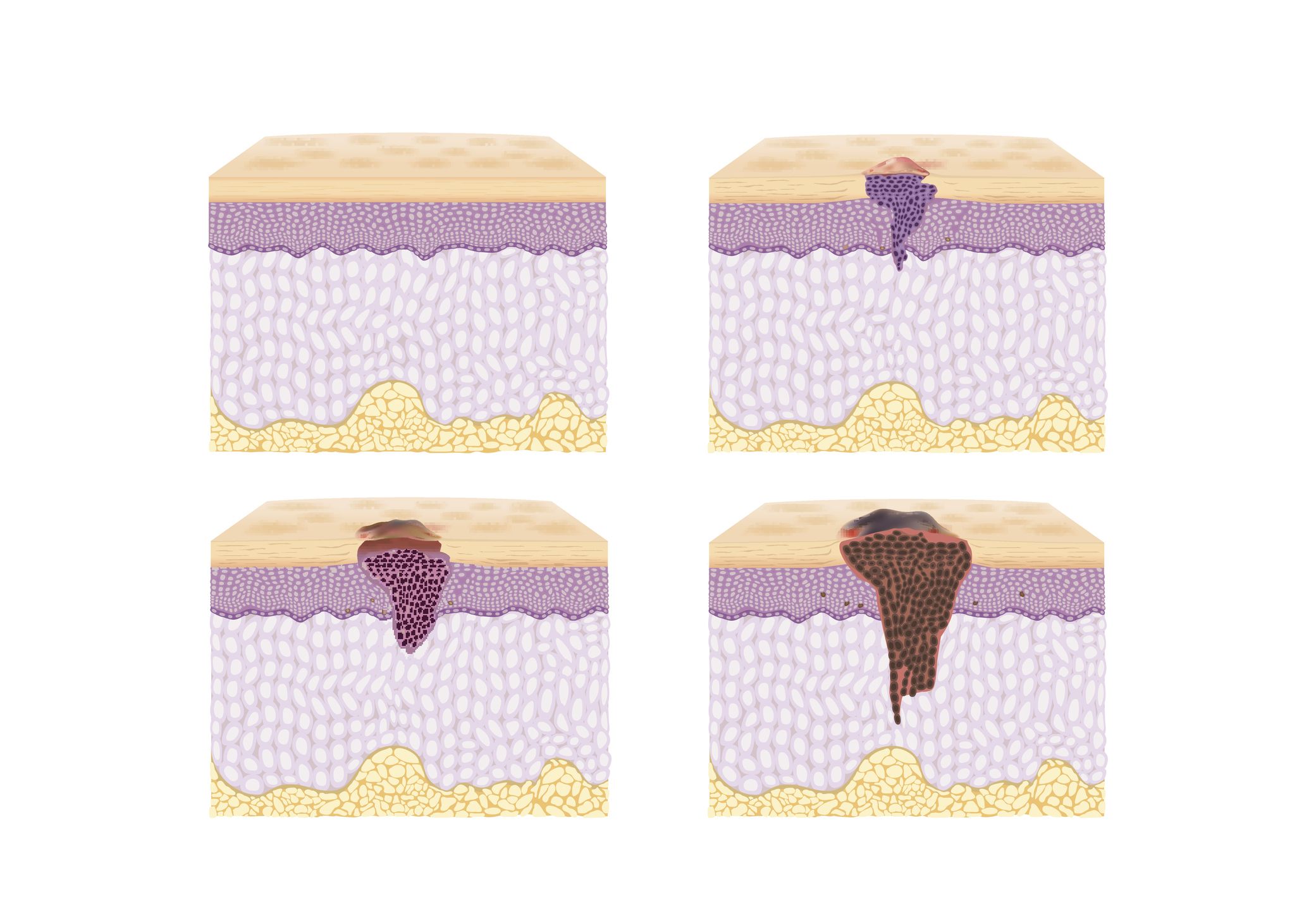
Simplified diagram showing the development of melanoma. The depth of penetration into the skin is decisive for the prognosis and further therapy.
- Top left: normal skin
- Top right: incipient melanoma in the upper layers of the skin
- Bottom left: Melanoma that has broken through the basal layer of the skin
- Bottom right: deep melanoma extending into the subcutaneous fatty tissue
How common is melanoma?
Malignant melanoma is the fourth most common type of cancer in Switzerland. In Switzerland, around 33 people per 100,000 are newly diagnosed with melanoma every year. In total, there are around 2,700 new cases per year in Switzerland. The number of new cases is increasing worldwide.
How dangerous is malignant melanoma?
Melanoma can be cured with surgery in over 80 percent of cases. However, in around 15 percent of patients it can form metastases in other organs. This leads to life-threatening situations. Cancer cells spread when they migrate via the lymphatic or blood vessels into the lymph nodes or internal organs and form new tumors there. The risk of this depends primarily on the thickness of the melanoma. The thicker (depth of penetration) the melanoma, the more likely it is to develop the ability to form offshoots. The faster the melanoma is treated, the thinner and smaller it is and the better the chances of survival.
Black skin cancer: causes and risk factors
The main cause of melanoma is UV radiation. You are exposed to UV radiation when you are in the sun or in a solarium.
Particularly at risk are people who:
- have a total of more than 100 moles (liver spots) on the body
- have fair skin (skin type I-II, i.e. reddish-blonde hair, blue eyes or freckles)
- Have cases of melanoma in the family
- have a weakened immune system, e.g. after an organ transplant or with an immunodeficiency disease such as HIV
- have already been diagnosed with melanoma in the past
- have suffered severe sunburns, especially in childhood and adolescence
Recognizing melanomas
It is important that you check your skin regularly. For patients with light skin types and moles in particular, it is advisable to examine the skin yourself at three-monthly intervals for suspicious skin changes. If you are unsure, consult a doctor. Also look at the hairy scalp, the back of the ears, the back of the neck and the genital region, possibly with the help of a mirror.
ABCD rule – skin cancer or birthmark?
The ABCD rule is a rough rule as to which moles should be checked more closely and shown to a doctor if necessary.
- A: Asymmetry: the dark skin spot is not circular, but uneven-sided
- B: Irregular border: the skin patch is not sharply demarcated from the surrounding skin
- C: Color: the skin spot is rather dark brown to black
- D: Dynamics: the skin spot has changed in a relatively short time
Treatment
Moles that change in shape, color or size should be shown to a dermatologist immediately. This also applies to those moles that are different from the others, that itch or bleed from minor injuries.
The aim of early detection is to diagnose skin cancer, and melanoma in particular, at an early and therefore easily treatable stage. At the University Hospital Zurich, we have a research focus on prevention and deal extensively with the early detection of skin cancer.
Online skin check: Quick and convenient from home
Send a photo of the affected skin area and fill out the short questionnaire. Within 24 hours on weekdays, you will receive a reliable diagnosis from our experts. Your data will be transmitted to us encrypted and treated confidentially.
Diagnosis of black skin cancer
Suspicious moles or spots are usually removed completely under local anesthesia (excision biopsy). The tissue is then examined under a microscope (histology). Once the diagnosis of melanoma has been made, further examinations such as an ultrasound of the lymph nodes or a whole-body examination using PET-CT are carried out, depending on the depth of penetration of the melanoma. Often the lymph node drainage is also examined and the sentinel lymph node is surgically removed. This also helps to identify small foci of offshoots, and further treatment is recommended if necessary.
New opportunities through innovative therapies
Melanoma treatment has changed considerably in recent years. Immunotherapy has brought significant progress. Medication is used to stimulate the patient’s own immune cells so that they can recognize the cancer cells and fight against them. Around 40 percent of melanoma patients with immunotherapy respond to this treatment and benefit from its high efficacy. Even in advanced stages of the disease, a cure is possible with immunotherapy.
Support immunotherapy with stool transplantation
There is strong evidence from studies that the microbiome, i.e. the entire microorganisms in the gut, has an influence on whether patients respond well to immunotherapy. In order to harness this effect for patients with a weak response to the therapy, a research project at the USZ is transplanting prepared stool from patients who have responded well to immunotherapy to patients with a weak or no response. In a pilot study, it was shown that transplantation improved the effect of immunotherapies in these patients with advanced malignant melanoma.
Personalized therapy with molecular genetic analysis
Tumors are complex structures, the cancer cells interact with the cells in the surrounding tissue in various ways. Viewed at the cellular and molecular level, every tumor and every cancer is therefore unique – there is no such thing as “the” lung cancer or “the” melanoma. If these individual differences from patient to patient are taken into account during treatment, therapies can be used in a targeted manner and with the greatest effect. At the same time, for example, drugs that only have side effects and no medical benefit in the individual case are excluded and – conversely – the risk that a promising therapy is not used is reduced.
Such individually tailored treatment is possible thanks to molecular genetic analysis. For this purpose, a tissue sample of the tumor is analyzed in the laboratory using a special procedure. The information from this study makes it possible to determine which of the available cancer drugs is likely to be most effective in an individual case. This targeted and rapid use of the most suitable therapy opens up new opportunities for patients who were previously considered to be out of therapy.