Overview: What is osteoporosis?
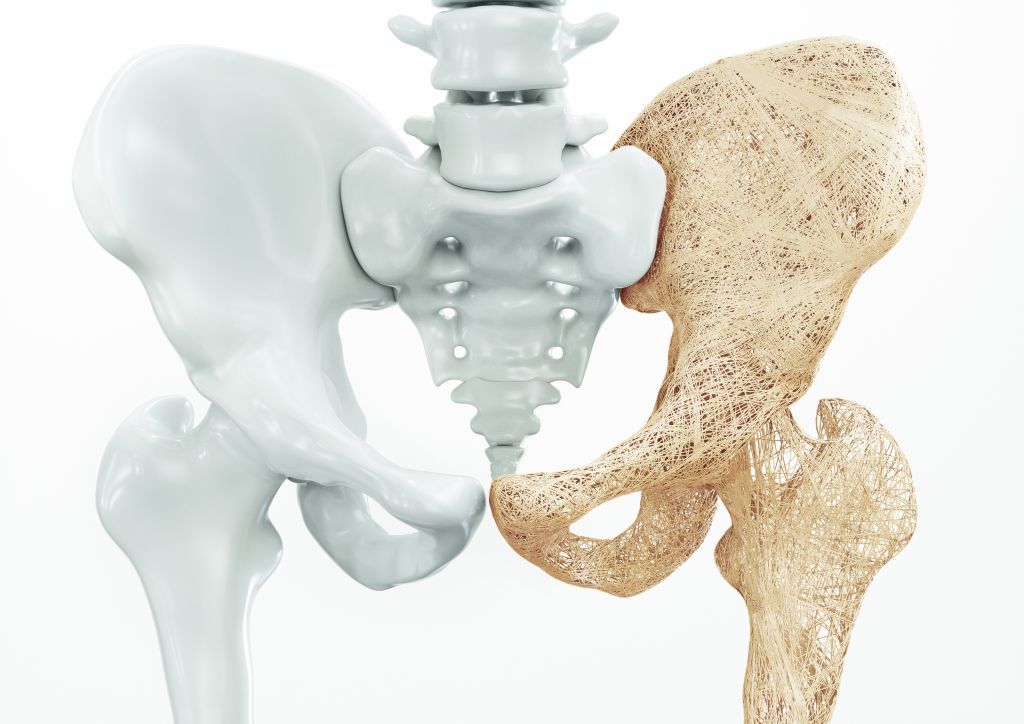
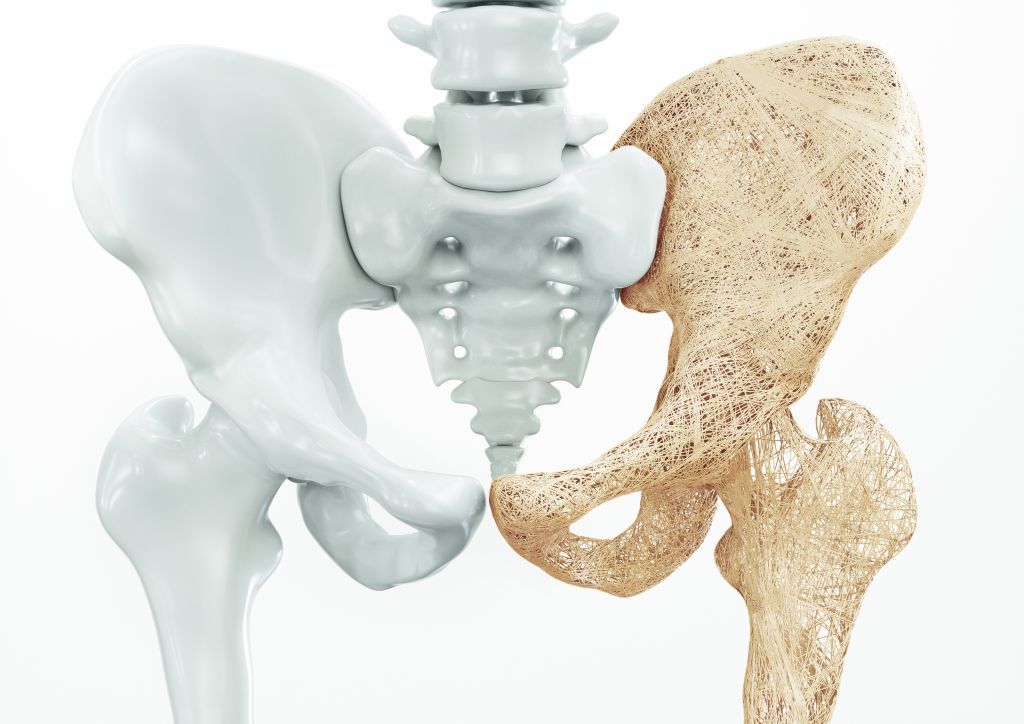
We build up our skeleton until around the age of 25. After that, our bones remain more or less stable for years. From the age of 40, the natural ageing process of our bones begins: The mineral salt content and thus the stability slowly decrease. In the case of osteoporosis, however, those affected lose too much bone mass in a short space of time. A healthy bone has a sponge-like structure with dense and firm structures, the bone beams. The decrease in bone density and the reduced bone quality leads to a decrease in the stability and resilience of the bones. If this process progresses, the slightest accident, everyday activities or even spontaneous fractures can occur. This often affects the spine, as well as the thighs, upper arms and forearms.
Although osteoporosis mainly affects women after the menopause, the disease can also occur in men at an advanced age. However, certain diseases or medication can also lead to reduced bone density in young people. Osteoporosis itself does not hurt, but bone fractures are usually painful and can lead to a loss of quality of life, especially in the case of hip or vertebral fractures. It is therefore advisable to start preventive measures at an early stage.
Osteoporosis: causes and risk factors
Various reasons can be responsible for the decrease in bone density and microarchitecture that ultimately leads to osteoporosis:
- Postmenopausal osteoporosis: This most common form of osteoporosis is caused by a lack of oestrogens (female sex hormones). Oestrogens regulate the female cycle and enable pregnancy. In addition, oestrogens also protect the bones and prevent them from breaking down, among other things. As less oestrogen is produced in the female body after the menopause, the risk of osteoporosis increases. Around 30 percent of women develop the disease after the menopause. If the menopause occurs before the age of 45, the risk of illness is also increased. Genetic factors can also favor the disease.
- Age-related osteoporosis: This affects both men and women equally and can set in from around the age of 70. Bone resorption has progressed to such an extent that the frequency of fractures increases.
- Secondary osteoporosis: Sometimes other diseases can trigger osteoporosis. In addition to rheumatoid arthritis, inflammatory bowel disease and diabetes, hormonal disorders (e.g. hyperthyroidism) and kidney disease are often responsible for the reduction in bone density and microarchitecture. Medication can also lead to osteoporosis. These include in particular cortisone, anti-epileptic drugs and anti-cancer drugs. Osteoporosis can also be seen in younger people.
Various other factors can increase the risk of illness:
- Lack of exercise and resulting muscle weakness
- Smoking
- Underweight
- Malnutrition with intake of too little calcium and protein
- Vitamin D deficiency
- Excessive alcohol consumption
Symptoms: Osteoporosis
In the early stages, there are hardly any noticeable signs of osteoporosis. A diagnosis at this stage is therefore only possible through a targeted search. If the disease is more advanced, bone fractures occur, which in turn cause discomfort. Depending on how and where the fracture occurred, pain can be acute or chronic.
The lumbar or thoracic spine is often affected. The associated pain is often diffuse and cannot be localized by those affected. Osteoporosis can also cause other symptoms:
- Size reduction of several centimeters
- Hunchback
- Fir tree phenomenon (the skin falls off in folds from the midline of the back to both sides)
- Reducing the distance between the pelvis and ribs
- Hollow back
Another frequently affected area is the hip. Hip fractures usually have to be treated surgically and often lead to a long period of restricted mobility and possibly a permanent need for assistance.
Osteoporosis assessment at the USZ
If the first symptoms or fractures occur that indicate osteoporosis, we will suggest an appropriate examination. It is also important to look specifically for osteoporosis in the presence of risk factors or certain other diseases. We use various diagnostic methods to detect osteoporosis:
- Measurement of bone density in the lumbar spine and hip, and possibly in the forearm: the T-value obtained in the so-called DXA measurement shows the deviation of the determined bone density from the average value
- Lateral DXA measurement of the spine for rapid detection of vertebral fractures (“vertebral morphometry”)
- Blood tests to detect other diseases and to check the nutrient supply
- Checking the risk factors
- Assessment of the risk of future fractures based on risk factors, physical examination, measurement results and laboratory tests
We can carry out additional tests to confirm the diagnosis:
The overall picture of the results enables targeted therapy.
Osteoporosis: prevention, early detection, prognosis
Although osteoporosis cannot always be completely prevented or stopped, there are various methods to prevent the disease. Many measures are easy to implement:
- Avoid smoking and alcohol: Smoking in particular robs the body of important vitamins and minerals and directly damages the bones. It is therefore advisable to avoid them altogether. Alcohol should also only be consumed in small quantities.
- Bone-friendly diet: A daily intake of around 1,000 to a maximum of 1,500 mg calcium is recommended. If possible, include calcium-rich foods such as dairy products, wholegrain cereals, pulses, green vegetables and mineral water in your diet. Sufficient protein is also important for normal muscle function and for maintaining bone stability. The daily intake should be around one gram per kilogram of body weight. An additional supply of nutritional supplements can also be helpful; we will prescribe these for you if necessary.
- Sunbathing: Vitamin D is needed so that calcium can be integrated into the bone structure. The human body produces this itself when exposed to sunlight. As a person affected, you can ensure the formation of sufficient vitamin D if you expose your face, hands and arms to the sun for several minutes without protection about three times a week. However, the sun is too weak in the winter months to enable sufficient vitamin D formation. An additional intake of vitamin D is therefore often advisable in consultation with your doctor.
- Weight regulation: If you are underweight, the body has too few nutrients and hormones available, which is why too little body mass promotes osteoporosis. Conversely, being overweight is a high stress factor for the joints and should also be avoided.
- Stay active: Regular exercise strengthens bones, muscles and your immune system – preferably in the fresh air. Strengthening training is particularly recommended to prevent osteoporosis and its consequences. All sports that put strain on the skeleton, such as dancing, skipping and hiking, also help to strengthen the bones. Balance and coordination exercises are also important.
If osteoporosis is not treated, bone density steadily decreases. Bone fractures can occur, especially in the spine, but also in the thigh and hip. The result is considerable pain and increasingly restricted life. As permanent pain is a massive mental and emotional burden, those affected should seek psychological support if necessary. Even if osteoporosis cannot be cured, the progression of the disease can be prevented or at least slowed down.
Self-help groups
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group is available from Selbsthilfe Zürich. Self-Help Zurich and the University Hospital Zurich are cooperation partners in the national project “Health literacy thanks to self-help-friendly hospitals”.
Osteoporosis: Treatment
Depending on the stage of osteoporosis, the aim of therapy is to stop or slow down the progression of the disease and to provide optimal treatment for existing fractures. The sooner you manage to eliminate possible risk factors and lead a healthy lifestyle, the sooner you can reduce or avoid the stressful consequences of osteoporosis.